05.10.16
Human factors in transfusion
Source: NHE Sep/Oct 16
Paula HB Bolton-Maggs, medical director of the Serious Hazards of Transfusion (SHOT), discusses the impact of human factors in blood transfusion and how errors can be reduced.
SHOT, the UK national haemovigilance scheme, published its annual report for events in 2015 in July this year. Since its inception in 1996 the most common adverse incidents in relation to transfusion are caused by human error, now more properly called ‘human factors’.
There is increased recognition of two important features: first that ‘to err is human’ or ‘we all do daft stuff’, and secondly that the environment in which we work, our training, staffing levels and work patterns all may influence how we make mistakes.
Rather than blaming the individual, every error in medicine can be examined to understand the contributory circumstances with a view to changing the environment (ergonomics) or other factors such as staffing. Human factors is now a recognised science. Errors are thought to contribute to death and morbidity across medical practice and not just in relation to transfusion, and recently were reckoned as the third leading cause of death in the US. Human factors training is now recommended and we need to learn to be situationally aware of the factors contributing to error such as multi-tasking, interruption and distraction.
Reports to SHOT demonstrate an increasing trend of organisational and staff factors contributing to breakdown of care, at worst linked to the death of the patient. Such factors include failures in continuity of care, multiple teams involved with poor handover, long shifts, and failure to escalate to senior staff when monitoring triggers high-risk scores. Reports of delayed transfusion with fatal outcome have increased and are usually multifactorial. For instance, several factors contributed to a complete breakdown in communication between a stem cell transplant unit and the associated transfusion laboratory for several months, resulting in inappropriate management of transfusion for several patients.
Reporting and feedback need to be improved
The NHS Staff Survey in 2015 demonstrated that less than half the respondents felt that their organisation treated staff involved in incidents fairly and only half reported adequate feedback. Recently multiple warnings have been given by senior Royal College representatives about the staffing crisis with insufficient staff to cover rotas in paediatrics, medicine and emergency departments. This has included using social media with the hashtag #mindtherotagap. All these factors increase risk to patients. It may be easier to blame an individual than to adequately address the surrounding organisational and staffing factors when people and resources are spread too thin. We talk about a blame-free culture, but the number of health professionals facing criminal investigation into ‘potentially avoidable deaths’ is increasing. These pressures contribute to a reluctance to report, and an exodus either to another country or early retirement with the loss of valuable experience, also evident in laboratory staff. Without a reliable and adequately staffed pathology service a hospital cannot function.
Near-miss incidents are very informative. One of the most dangerous errors in transfusion is the inadvertent transfusion of an ABO-incompatible unit of red cells (a ‘never event’). About 10 of these are reported each year but only a third of these are associated with harm or death. These serious incidents have resulted in staff dismissals and/or criminal prosecutions. A review of all never events noted that reporting in hospital quality accounts ‘is neither consistently transparent nor adequate … the true root cause is likely to be organisational rather than individual’, further evidence of failure to engage with the human factors that underlie these mistakes.
Near-miss incidents comprise a third of the 3,500 or so SHOT reports each year; most of these are instances of blood sampling from the wrong patient. In 2015, we noted that there were at least 288 instances where a wrong blood sample could have resulted in an ABO-incompatible transfusion if it had not been detected. Most were detected because a previous sample gave a different blood group. These wrong samples are most often taken by medical staff and occur mainly because the patient has not been properly identified and/or the blood sample is labelled away from the patient. The ratio of such near miss to actual wrong transfusions is about 100 to one.
Recommendations from SHOT
Recognition that we have not had much impact on these errors in transfusion over the last decade has resulted in detailed human factors analysis of some cases reported to SHOT which display failures of communication, exacerbated by shift patterns and lack of continuity of care in hospital practice. These issues are not peculiar to transfusion but are seen across medical practice and other factors in the patient journey contribute to transfusion adverse outcomes.
Blood transfusion involves nine steps each of which may be completed by a different healthcare professional. In both 2015 and 2014, 78% of all incidents analysed by SHOT were error-related. Only 10% were not preventable (e.g. acute allergic transfusion reactions which are idiosyncratic). An additional notable feature is that in the nine-step process transfusion errors are frequently multiple (median number three). Identification of the correct patient at the time of blood sampling and at the time of transfusion is key, yet staff make assumptions and take shortcuts, and then do not perform this positive patient identification correctly. There are some parts of medicine where a checklist is essential, and SHOT recommends a five-point bedside checklist as the blood component is attached to the patient. This would prevent deaths and other serious complications.
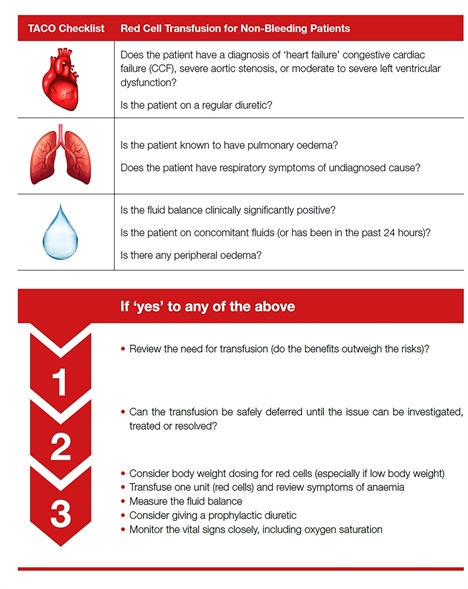
The greatest number of deaths and serious harm in transfusion result from pulmonary complications (55% over the last six years), most commonly related to transfusion-associated circulatory overload. Many of these cases might be prevented by more thorough pre-transfusion assessment and single unit transfusions followed by reassessment. The second recommendation from SHOT this year is a checklist and tool for this .
Our advice is to be WARM – Work Accurately and Reduce Mistakes. Blood components are now very safe but our practice needs improvement. Despite this, transfusion remains very safe in the UK with a risk of death where the transfusion was contributory of approximately one in 100,000 components issued.
FOR MORE INFORMATION
W: www.shotuk.org