01.04.15
Health coaching in the east of England: promoting patient centred care and behaviour change for people with long-term conditions
Source: NHE March/ April 15
In 2012, Andrew MacPherson and the Strategic Projects Team were asked to support an innovative idea that was struggling to get off the ground, despite having all the hallmarks of a simple solution for radical change in healthcare delivery. Dr Penny Newman, a GP, consultant in Public Health and director of Service Integration at Colchester Hospital, and co-creator of the Health Education East of England Health Coaching Programme, explains more.
The considerable and increasing impact of long-term conditions (LTCs) on morbidity, mortality, quality of life and healthcare costs is well known. Poor, avoidable health behaviours account for 60% of deaths.
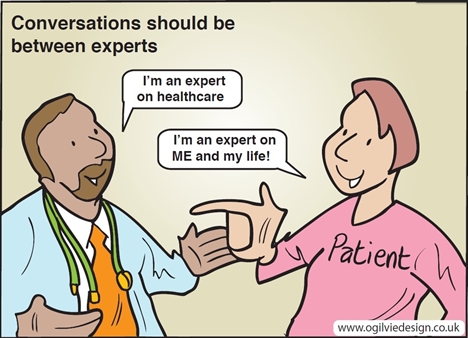
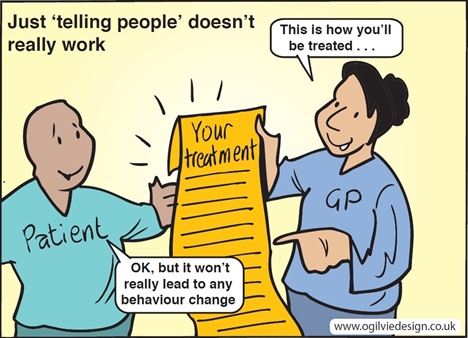
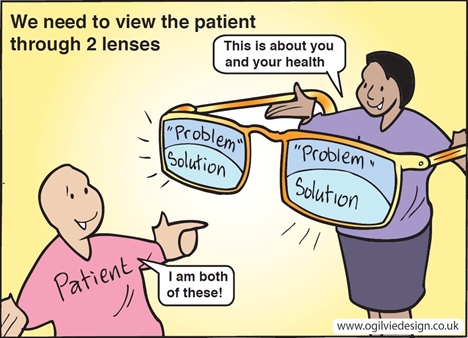
Helping patients thrive in the presence of disease requires a paradigm shift in the way clinicians work with them. This means moving away from a paternalistic and dependent consultation model of ‘fixing’ to one that is empowering and where responsibility is shared with patients and their carers.
Health coaching is a different way of relating to, and talking with, patients. It is patient-centred and supports self-management and behaviour change. Together with population approaches, this shift in consultation style can increase patient activation, confidence, compliance and healthy behaviours – which are all needed to improve outcomes and reduce healthcare costs. It delivers on the commitment in NHS England’s Five Year Forward View and the need to tap into the ‘renewable energy’ of patients and communities.i ii iii
What is health coaching?
Health coaching is a patient-centred process based on behaviour change theory, which entails patients setting self-determined goals. It is one of many ways to support self-management and can be delivered either alone or aligned with other elements, e.g. augmenting care planning and clinician activation – two elements of the new NHS LTC delivery system, ‘The House of Care’.iv
Although an innovation in the UK, health coaching is used throughout the USA to provide self-management support to people with LTCs, to aid decision making, and to improve lifestyle and medication compliance. There, it is delivered by a range of providers who offer health coaching to private individuals alone and as part of health programmes and systems.v
A recent systematic review has led to a consensus definition which outlines the change in roles between patient and clinician central to this approach:
A patient centred approach wherein patients at least partially determine their goals, use self-discovery and active learning processes together with content education to work towards their goals, and self-monitor behaviours to increase accountability all within the context of an interpersonal relationship with a coach. The coach is a healthcare professional trained in behaviour change theory, motivational strategies, and communication techniques, which are used to assist patients to develop intrinsic motivation and obtain skills to create sustainable change for improved health and wellbeing. (Wolever RQ, 2013)
Health coaching is undertaken by health professionals or people with LTCs (peers) and can take place in-person, by telephone, email or online, or using a combination of approaches. It may be one-off or may occur regularly, such as every week or month for several months.
Health coaching in the East of England
Health coaching in the East of England integrates a health coaching approach into core consultation skills and hence is delivered as part of a patient’s usual care.
In 2010, I attended executive coaching training run by The Performance Coach. Recognising the value of coaching with my patients, with Dr Andrew McDowell I then designed and piloted health coaching training in primary care in NHS Suffolk, supported by an East of England Regional Innovation Fund (RIF). After a positive evaluation,vi and with commercial guidance from the NHS Strategic Projects Team and funding from Health Education East of England, the programme was rolled out in March 2013.
All organisations across the region were invited to nominate clinicians to attend a two-day health coaching programme. Two ‘train the trainer’ programmes were run, consisting of six days of training and four days of co-delivery to develop an internal training resource in the region.
From April 2013 to March 2015, almost 800 clinicians were trained in multi-disciplinary groups. They came from 45 organisations, including acute trusts, community services, county councils, mental health trusts, CCGs and general practice, and 20 internal trainers were accredited. Participants included nurses (44%), allied health professionals (28%) and doctors (9%).
The training offered was delivered in a coaching style and highly experiential. It included theory and practice in the foundations of coaching and behavioural change techniques that could be integrated with, and build on, clinical and consultation skills.
Benefits to patients, clinicians and the NHS
Evaluation included post-training surveys, a qualitative evaluation by The Institute of Employment Studies (IES) and a rapid review of the literature by the Evidence Centre.
In the surveys, more than 96% of clinicians rated the content, delivery, learning opportunities and application to their work as ‘good’ or ‘very good’. They said a coaching and patient-centred mindset was applicable to all patients, and that skills in behaviour change were applicable to patients requiring lifestyle change, with applicability to those with single or multiple LTCs, for some mental health problems, for rehabilitation, palliative care and to improve medication compliance.
The qualitative evaluation involved focus groups, interviews and organisational case studies including CCGs, hospitals and GP surgeries. Overall, clinicians perceived the two-day training intervention as effective, with high levels of usage. Organisational culture and work context were key success factors, with greater local support ensuring transfer of learning to daily roles.
As one GP put it: “The biggest thing for me was the shift in my mindset from the ‘doctor knows best’ approach, to where the patient is the ‘expert’ of their own life, and already has the means within themselves to improve their own health and life experience.”
Two-thirds of clinicians were using health coaching with a wide range of patients and conditions (depression, weight, smoking, foot ulcers, pain, anxiety, COPD, coronary heart disease, poor kidney function, hypertension) and finding it useful.
The reported benefits in NHS efficiency and effectiveness included higher patient compliance; reduction in episodes of care; reduction in appointments per patient; improved quality and consistency; quicker discharge of caseload; potential to cut waiting list times and for less acute admissions; less waste from unnecessary tests and medication.
Reported benefits to patients included increased confidence; increased patient empowerment; more personalised advice/care; reduced dependency; increased satisfaction and less medication.
A case study indicated a 63% indicative cost saving from reduced clinical time, compared to usual non-health coaching approach, giving a potential annual saving of £12,438 per FTE if reduced clinical time was widely replicable and sustainable over time.

A review of evidence
The (mainly US) literature on health coaching is difficult to interpret given poor definitions of health coaching and design, and hence it is difficult to compare studies and generalise to the NHS. The 275 studies included in the review show, importantly, that health coaching works best for people most in need. This includes people with low levels of self-efficacy, those at highest risk, those with the most severe symptoms, with low levels of self-management or medication adherence, women, young people or much older people, minority ethnic and vulnerable groups, and people with the lowest levels of education. Health coaching can support patients’ motivation to self-manage and adopt healthy behaviours, is widely applicable and can be adopted by all professionals and peer coaches.
Next steps
Health coaching is an innovation and early feedback from the programme indicates it is highly popular with clinicians and can help organisations meet the challenges of improving quality, communication and patient experience, and potentially reduce demand and costs. It supports strategies for improving the management of LTCs and frail elderly patients, as well as promoting better integration of services around individual patient’s needs.
Health coaching straddles leadership and clinical training, and as an educational intervention can be an enabler in service transformation. It is a route into developing clinical leadership as skills are transferable, e.g. to appraisal and performance coaching.
In this challenging NHS environment, new and innovative approaches are urgently required. Health coaching needs further development, including an evaluation of the most cost-effective methods of training clinicians, and patient outcomes.
However, evidence so far suggests that – if sustained – this ambitious programme could produce a paradigm shift in the mindset and behaviours of professionals to support behaviour change, and reinforce a more empathetic and person-centred experience for patients.
We are grateful to Karen Bloomfield, leadership and organisational development manager, and to Health Education East of England for the invaluable support and collaborative leadership in the programme.
Testimonials from health professionals who have tried this approach
Children's Community Occupational Therapist: “I work with children with chronic fatigue and their parents. My colleague and I have noticed that there is a lot of 'learnt helplessness' which quite a few families have developed in contact with professionals. We are re-organising our service now and planning to base our service on the 'philosophy' of health coaching - providing the information needed and then try and develop goals with the young person (and parent) and impart the idea that they have the responsibility and power to influence their own health…I think that our whole team of OTs and Physios should be trained in health coaching and I would love to do this."
GP: "I really love this model of consults with patient and it has fired me up to want to be a coaching trainer so that I can disseminate these easy-to-learn, but incredibly powerful techniques with their own patients. The biggest thing for me was the shift in my mind-set from the 'doctor knows best' approach, to where the patient is the 'expert' of their own life, and already has the means within themselves to improve their own health and life experience."
Clinical Research Nurse: "I was visiting a depressed patient and his wife who are on one of my stroke studies. On arrival, the patient was very negative and despondent, but on using the coaching to set a goal, he became very animated, and started coming up with all sorts of options for himself to try out. I listened more, and as a result, he worked it out for himself."
Community Physiotherapist: “I deal with patients who have long-term conditions and associated complex needs. The particular case I am referring to, involves a gentleman that is a persistent faller as he is not able to move independently without prompting from his wife. The health coaching approach was carried out with this gentleman to explore the benefits of walking daily to promote continued exercise tolerance, maintain cardiovascular fitness and prevent learned immobility. The raised awareness of the patient has enabled him to be discharged to self-manage and it is clear how to discuss patient’s potential with the wider MDT when they try to refer back for the same issues. The coaching approach enabled a light bulb moment for the patient with his response being 'I have the answers; it's down to me to keep to my plan'."
Practice Nurse / Respiratory Nurse Lead: "I have a patient with COPD who smokes. Usually I would say 'you really should stop smoking'. This time I asked: 'What do you think would make your chest better', and the patient immediately identified stopping smoking. She set the goal to stop realistically after her birthday in two weeks’ time, looked at her options and decided to go to level 3 group as she wants to go to a class. She will see me a week after the class for coaching. She is delighted and so am I, as the idea came from her not me."
Summary of the Health Coaching approach in the East of England
|
Aims to
|
- Increase health-related quality of life and outcomes
- Improve patient experience of the health system
- Ensure best use of services and reduce cost
|
|
Supports a person to change their relationship to their health
|
- Realises potential and supports self-management
- Raises awareness and sense of responsibility
- Increases confidence and motivation to act
|
|
Health Coaching Competencies for clinicians
|
- The application of a patient centred approach built on empathy and rapport
- Managing self and believing in patients potential to self-manage to create shared responsibility
- Enhancing core skills and developing a flexible consultation style
- Establishing patients’ self-determined goals and action planning
- Managing the process and relationship including use of behavioural change techniques
- Integrating clinical expertise with interpersonal skills in behaviour change
- Reflecting on effectiveness and considering the impact of/on the wider system and resources.
|
|
Requires a different kind of conversation
|
- Tailored to the individual, their agenda and goals
- Based on listening, trust, challenge and positive emotions
- Is collaborative and equal
- Requires transformation in the clinician/patient relationship
|
|
Useful in
|
- Improving lifestyle
- Chronic disease management
- Pain management
- Mental health (primary care)
- Medicines management and optimisation
- Decision support
- Recovery and rehabilitation
|
|
Benefits
|
- Improved patient satisfaction and self-efficacy
- Creates a mind-set shift & resilience amongst clinicians as they move from expert to enabler
- Some experience of reduced service utilisation and improved outcomes
- Creates clinical champions for spread
- Use for behaviour change, all consultations and with colleagues (triple benefit).
|
|
Contributes to organisational priorities
|
- Improved patient experience and communication
- Quality of care
- Integrated care
- Management of long term conditions
- Reduced complaints
|

Above: Dr Penny Newman
References
i. Fenk J, Chen L, Bhutta Z, Cohen J, Crisp N, Evans T, Fineberg T, Garcia P, Ke Y, Kelley P, Kistnasamy B, Meleis A, Naylor D, Pablos-Mendes A, Reddy S, Scrimshaw S, Sepulveda J, Serwadda D, Zurayk H. (2010) Health Professionals for a new century: transforming education to strengthen health systems in an interdependent world. The Lancet (376) 1923-1957
ii. Naylor C, Imison C, Addicott R, Buck D. Goodwin N, Harrison T, Ross, Sonola L, Tian Y, Curry N (2013) Transforming our Healthcare System. 10 top priorities for commissioners Kings Fund
iii. Juddith Hibbard, Helen Gilburt. Supporting people to manage their own health. An introduction to patient activation. Kings Fund. May 2014.
iv. Coulter A, Roberts S, Dixon A, (2013) Delivering better services for people with long-term conditions : Building the House of Care, Kings Fund
v. Moore M (2013) Health Coaching Summit. NHS Institute. Video recording from conference Westminster Hall 26th February 2013.
vi. Thomas W, Primary Care health Coaching Evaluation Report Executive Summary University College Suffolk, 2011.
FOR MORE INFORMATION
E: [email protected]
E: [email protected]
E: [email protected]
W: bit.ly/health_coaching
W: www.thestrategicprojectsteam.co.uk