01.02.15
Mobile phones are vital to the future of European healthcare
Source: National Health Executive Jan/Feb 2015
Jonathan Seddon and Wendy Currie of the Audencia Nantes School of Management, France, discuss the practical benefits of mobile health, also known as mHealth.
Europe’s health systems are facing many challenges. People are living longer (by 2050, the average life expectancy in Europe will be 82.5), chronic illness is increasing (the number of patients suffering from diabetes, heart disease, cancer and dementia is growing), and hospital budgets are struggling to keep up with increasing pressures.
One solution is the integration of mobile technologies, hospital services and patient data, underpinned by changes to each government’s digital strategy and telecommunications investment. Healthcare resources are concentrated in regions with the highest population, so the ability to access medical information in rural areas will extend the benefits of mobile health to greater numbers of citizens.
Through the consolidation of health records and patient data into cloud services, patients will benefit from health applications delivered via their mobile devices. In a recent survey published by the authors, the digital divide across Europe continues.
Whilst each country has between 99% and 100% of its population covered for 3G phones, this is not the same for advanced fourth generation mobile broadband availability (4G LTE protocol). Here, those countries that have stronger economies and higher GDP, (e.g. Italy, Spain, Poland, UK, France, Germany, Finland and Sweden), have more than double the coverage that is available in the rest. With the exception of Greece, between 2005 and 2012, every European country has increased its volume of mobile traffic. However, this has not been equally enjoyed by all of the countries, because the cost of these services varies. Clearly, where the costs are high, the less time an individual has to spend on the internet.
An online service index (OSI) has been calculated by the UN in an attempt to allow objective comparisons on how each country’s government has used the internet to deliver its policies. This calculates differences in each country’s development of eGovernment and includes measures for the provision of information, online services, eProcurement and mobile government. Such an index has again highlighted which countries have invested in eGovernment services – reinforcing the difference between developing a web site that allows individuals to seek health information with one that offers the ability to book appointments and securely exchange information with others.
Whilst there are increasing trends across Europe to access medical information via the internet, doing so via a mobile phone can vary widely between countries. For example, in 2012 over 46% of Swedes utilised mobile internet, whilst this figure was just 1.9% in Bulgaria. So having an eGovernment strategy is not enough to encourage citizens to use these services.
We identify four different mHealth scenarios shown in Figure 1 (© Currie and Seddon 2014).
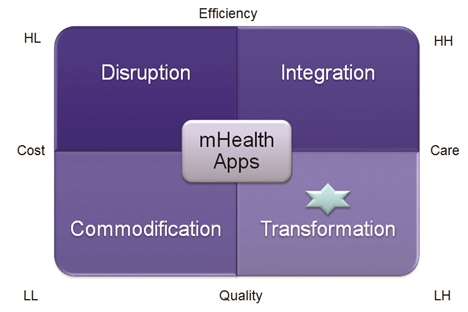
Commodification
There are more than 100,000 mobile health apps on the market, and citizens may download them at no or low cost. Many are low quality, with limited benefits for citizens. Currently, citizens are confused about the mobile health market, so government and healthcare managers need to develop effective education and training programs.
Disruption
The legal and regulatory environment is uncertain. Providers of mobile apps may be faced with high costs where mobile app service delivery results in fines and penalties, e.g. due to citizen data infringement. Current EU and US regulation is a work-in-progress, yet the potential for disruption of the health industry is huge.
Integration
Enhanced quality and efficiency to stakeholders from mobile health is likely to occur when patient data is integrated across different clinical and non-clinical systems. Integration will significantly raise costs in the short-term, particularly where traditional health systems are replaced with new ways of providing mobile health (e.g. fewer visits to the surgery, or better monitoring of patient conditions using smartphones).
Transformation
The best-practice scenario is where mobile health can transform health systems without significantly raising costs, while also improving care. Technology is only one factor in health system transformation. Economic, social and cultural factors are also important, and governments need to play a significant part in protecting citizens with new laws and regulations to keep pace with fast moving technologies.
Healthcare managers are facing extremely challenging conditions. Our research suggests that mobile health offers many potential benefits, but it is clear that health systems will need to undergo changes as a result. As life expectancy increases, along with the growth in chronic conditions, health tourism is likely to increase – where citizens seek better diagnoses, treatments and cures for a range of health conditions. The notion that citizens will only receive health services in their country of residence will become less likely.
Mobile health will fuel this trend, but healthcare managers will need to plan to integrate health and social services to move mHealth from its current commodity status to one where health service delivery is transformed for the benefit of all citizens.
Tell us what you think – have your say below or email [email protected]