30.11.15
The service user perspective
Source: NHE Nov/Dec 15
 Fabia Holt, research and consultation lead for the Department of Health ProCure 21+ Repeatable Rooms initiative, explains why it is important to involve those who are actually going to use NHS facilities when designing them.
Fabia Holt, research and consultation lead for the Department of Health ProCure 21+ Repeatable Rooms initiative, explains why it is important to involve those who are actually going to use NHS facilities when designing them.
Over the past year nearly all discussions within and about the NHS have featured some aspect of crisis, mostly in response to an ‘affordability gap’ of £30bn by the end of the decade.
Of the £110bn annual turnover of the construction industry, 40% comes from the public sector, and at present the NHS is the largest capital construction client in the country. NHS capital projects have been a target of cost reduction savings to the tune of 20%.
The ‘P21+ Repeatable Rooms and Standard Components’ programme
The ‘P21+ Repeatable Rooms and Standard Components’ programme has been developed in response to this, with the aim of driving cost efficiencies by standardising design and identifying opportunities for bulk-buying within the NHS.
This seems an unlikely introduction for an article on strengthening the service user voice, and yet the Government Construction Strategy is where the journey started. The P21+ team developed a ‘repeatable mental health bedroom’ that has delivered cost efficiencies while improving the service user environment.
In developing a ‘repeatable mental health bedroom’, the P21+ team followed a robust design process that tested and re-evaluated assumptions. This included a literature review, an evaluation of existing designs, peer reviews and mock-up tests.
During 2014, the team also visited NHS trusts across the country and mental health support groups, including the Mental Fight Club in Southwark and Innovate Dementia in Merseyside, to understand current issues and identify ways to improve the design of mental health facilities.
Initial consultation findings
The most heated debates for staff were centred on the extent to which the design should maintain patient safety – estates managers usually argued that the design should not accommodate any risk, despite the impact on privacy and dignity. Nurses often disagreed and felt that risk should be managed operationally wherever possible.
Staff questioned the functionality of different spaces and the impact on both care and staffing. Although a TV and easy chair can put service users at ease, providing these facilities in the bedroom encourages isolation, which can be detrimental to recovery and challenging to staff.
Service user support groups indicated that rooms are stripped of identity, with no stimulation to help users connect to the outside world. With only four blank walls to look at, service users felt there was no hope of the environment helping recovery.
Design solutions
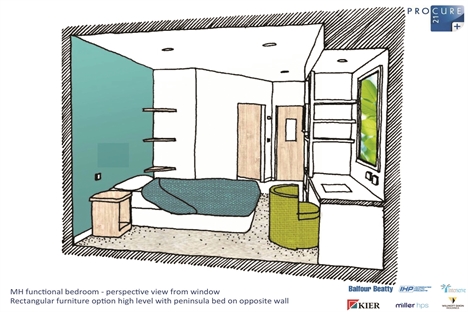
The team used a range of sketches (one of which is pictured above) to get feedback from service users on design ideas.
The site visits enabled the team to see examples of innovation, including the use of different flooring at the entrance with a coat-and-shelf unit to create a threshold that acted as a lobby.
Participants at the Mental Fight Club felt that furniture too often dominated bedrooms, with floor-to-ceiling shelves rather daunting; a desk can be an unwelcome reminder of work pressures. The group made the design team consider what the bedroom feels like when items are not used; when large shelving units are left empty or when a noticeboard has no pictures. The design team suggested a noticeboard with a background picture to add colour to the room and responded to the group’s calls for storage to be broken up into more manageable spaces around the room.
By positioning the bed opposite the TV, the design encourages service users to lie in bed and perhaps fall asleep watching TV. Placing a chair in front of the TV was preferred as this enables active viewing and differentiates functions within the room.
The design solution the team created includes a window seat, and when this was spotted, one participant captured the group’s response when he said: “Nothing else in the room would matter if I had a window seat, I’d spend all my time there.”
A window seat provides a private space and an opportunity to connect to the outside world.
Participants felt the design should be a reflection of how they should be treated and therefore the design should be as normal as possible, with anti-ligature fittings fading in (rather than dominating) the design.
Conclusion
The ‘Repeatable Rooms and Standard Components’ programme has achieved target cost savings of up to 14.1% and has been implemented at Scarborough Hospital (see case study below) and the Royal Stoke University Hospital. The programme has demonstrated that NHS trusts can make significant savings while improving the patient environment.
(Image credit for this image and top image: Rosemary Jenssen / Jenssen Architecture)
About the author
Fabia Holt is a highly-skilled project manager and healthcare planner who works predominantly in the health sector at Sweett Group. She is completing an MSc in Construction Project Management and has lectured at London South Bank University on ‘Planning Buildings for Health’.
Repeatable rooms case study: Scarborough Hospital, York Teaching Hospitals NHS FT
Source: www.procure21plus.nhs.uk/repeatable-rooms-and-standardised-components-achieves-clinical-and-cost-efficiencies-at-scarborough-hospital/
A £4m surgical ward new-build project at Scarborough Hospital has incorporated two repeatable room designs and several Standardised Components from the ProCure21+ Standardisation programme, saving over £90,000 and allowing a further facility to be built as part of the original capital project, it was reported in October 2015.
Time and programme savings have also been significant, according to trust capital projects programme director James Hayward: “We had calculated on savings in the planning and construction phases as a direct result of using the Standardisation rooms and components, but we were very pleased to find that the benefits were tangible in the design phase, and now in the operational phase of the building’s life as well.”

Evidence-based and tested
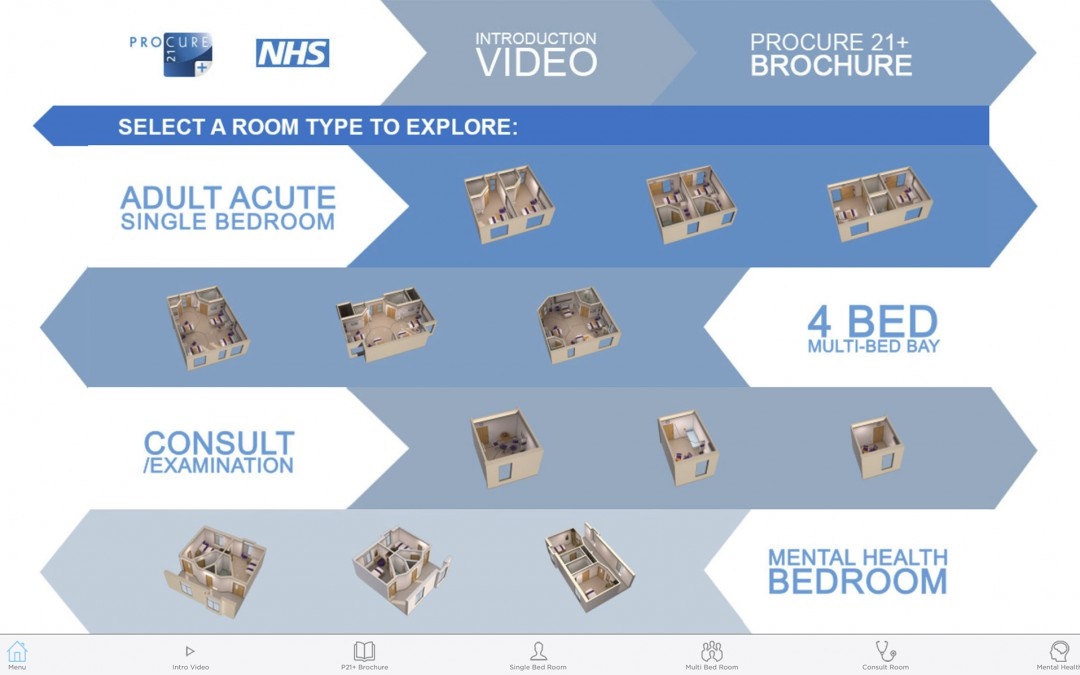
The Repeatable Rooms and Standardised Components initiative is part of the Department of Health’s Cost Reduction Programme for capital schemes within the NHS. The initiative began in 2013 following a Department of Health conference at which 95% of NHS trusts present voted to develop a set of evidence-based room designs that could be repeated across a new-build or refurbishment project. The development process was “short but very intensive” according to programme director David Kershaw: “We began in 2013 by conducting a thorough review of the evidence-base to determine best design practice for a number of acute rooms, including a single-bed room with en-suite, a consult/exam room and a multi-bed bay that could be repeated to form a ward. An evidence matrix was drawn up, showing correlates between design parameters and patient/staff experience.”
Following this, patient group representatives were invited to share their experience, and exemplars of good design from all procurement routes, including internationally, were added to the evidence matrix. Room designs were drawn up and subjected to expert panel reviews including representatives from the NHS, the construction industry, Royal Colleges and patient representative organisations, with feedback incorporated in the designs. In a rigorous test series, real-life processes were carried out in full-scale mock-ups of the room designs. BIM models were federated and costed before the room designs and components were rolled out in early 2014. The process was then repeated for mental health environments, leading to two repeatable room designs for functional and organic mental health users. Development is now well advanced for repeatable high- and low-acuity treatment rooms and a chair-centric space for emergency departments.
New ward capacity
The Scarborough programme delivered 17 single rooms and four four-bed multi-bed bays, with two treatment rooms designed and built to the same size and configuration as the single rooms: “If activity and demand patterns change, we can convert one of them back into a single room,” says Hayward. Standardised components used were doors, windows, interstitial blinds, doorframes and M&E components such as lighting and ventilation.
While the trust had anticipated some of the eventual operational-phase benefits of incorporating the Standardisation programme – including infection control benefits, efficiency of footprint and the resulting clinical efficiencies – the planning team were surprised at how quickly the benefits were realised during the planning and design stage. “For instance, we saved 60 clinical hours because we were able to present one room for approval to the clinical team and then deliver 17 of them with no further need for consultation,” says Hayward. “The designs were proven and backed by evidence and that was a conclusive argument in their favour. Plus, the rooms were already available as fully loaded BIM models, so we could walk clinicians through a virtual space and they could understand easily what it would look like and how it would work.”
Kier Health’s ProCure21+ framework manager Robbie Blackhurst said there were also cost savings at the design stage: “Because we were implementing a set of approved layouts with defined clinical benefits, it expedited agreement of the 1:200 design, allowing us to achieve clinical sign-off with only one iteration required at that stage. That resulted in a 7% cost saving, which was taken straight off the bottom line.”
More on the background to the project and its successes at the ProCure21+ website.
Source: www.procure21plus.nhs.uk/repeatable-rooms-and-standardised-components-achieves-clinical-and-cost-efficiencies-at-scarborough-hospital/