23.11.15
Agency pay cap comes into effect today
Monitor and the NHS Trust Development Authority (NHS TDA) have introduced caps on the hourly rates paid for all agency staff, which take effect at midday today (23 November).
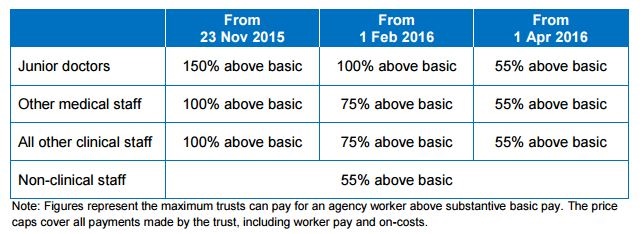
The price caps will apply across all staff groups – doctors, nurses and all other clinical and non-clinical staff – but will ‘ratchet down’ subject to monitoring on 1 February 2016 and 1 April 2016.
In a letter to all NHS trusts and NHS foundation trusts employing agency staff, the regulators stated that the latest financial performance, which revealed the NHS has racked up a £1.6bn half-year deficit, highlights the need for “concerted further action” on finances in 2015-16, particularly to tackle the rapid growth of spending on agency staff.
The regulators added that the new hourly price caps will build upon the new framework system that that has been launched to ensure only agencies provide quality staff at a price that is value for money can provide nurses to the NHS and the introduction ceilings on the numbers of agency nurses.
The following table summarises the trajectory of the price caps:
Following the price cap consultation, Monitor and NHS TDA have decided not to include bank workers’ pay under the price cap rules.
They said: “We will keep this under close review and if bank pay rates increase substantially, we will move to extend the price caps to bank workers.”
All trusts are required to report to Monitor and TDA when they exceed the price caps.
Saffron Cordery, director of policy and strategy at NHS Providers and a member of the NHE editorial board, said the implementation of hourly price caps for all agency staff and a cap on management consultancy spend has the potential to be a key part of returning the NHS to financial balance.
“It is important that the regular monitoring process is implemented in a proportionate manner with minimum administrative burden so that the NHS frontline can focus on continuity of high quality care for all patients and service users,” she stated.
“The success of the price caps will depend on all providers adhering to them so it is positive that Monitor and the TDA have listened to and responded to consultation feedback from providers.”
But Janet Davies, CEO and general secretary of the Royal College of Nursing, added that the NHS needs an urgent cash injection.
“If the government hopes to solve this financial crisis by capping agency spend, it will be disappointed. This crisis was not caused by agency staff,” she said. “While it is right to reduce the money spent on short-term staffing, this should be done by increasing the supply of long-term staff, by training more nurses and paying them fairly.
“The government must give the NHS the money it needs now, and make it easier for trusts to provide safe staffing in a sustainable way in the long-term. The government must act now to protect patients.”
Tom Hadley, director of policy at the Recruitment & Employment Confederation (REC), described the decision to introduce the caps, just five working days after the close of the official consultation, as “illogical”.
“As of today, doctors and nurses who provide crucial front-line services to NHS patients – often at short notice and during unsociable hours – are having their pay cut,” he said. “This cannot be right and with increased winter pressure on the NHS soon to come, it puts patients’ health at risk. This policy will drive skilled professionals out of the NHS and make the current staff shortages even worse.”