03.10.16
Operational plans timetable ‘extremely challenging’ for providers
NHS Improvement has warned that it will be ‘extremely challenging’ for trusts to complete operational plans to support their sustainability and transformation plans (STPs) for next March.
All NHS trusts and FTs are required to produce two-year operational plans for 2017-18 and 2018-19 that are consistent with the goals of their area’s STP, and will allow providers to at least break even.
Trusts are required to submit their draft plans on 24 November. They must then be approved in time for the national deadline for signing contracts on 23 December.
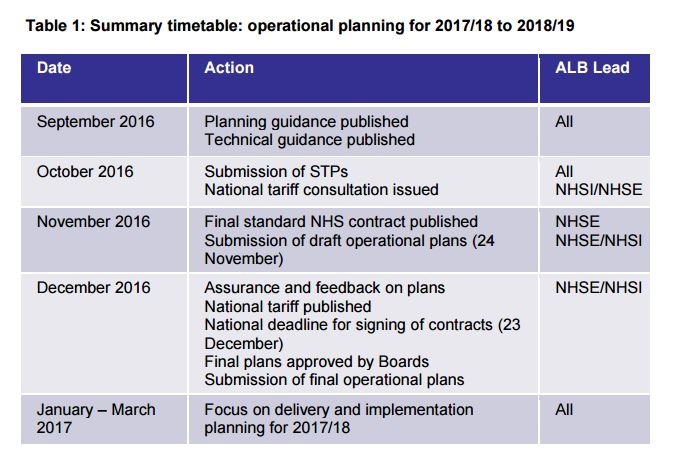
A report from the NHS Improvement board meeting on 29 September notes that this is a significantly shorter timeline than allowed for the previous lot of plans, which were prepared between January and March 2016.
NHS Improvement is now developing a streamlined process for plan assurance to help ensure the plans are delivered on time.
NHS England recently published its first two-year operational planning guidance to try to make the planning process easier for trusts.
Dr Graham Jackson, co-chair of NHS Clinical Commissioners and chair of NHS Aylesbury Vale CCG, warned at the time that the timescale was challenging, and that the two-year contracts would create a risk of “unsatisfactory results” if the decision-making process was “rushed”.
The board papers also say that all STPs have now produced two-page plans for implementing the recommendations in the Carter Review regarding pathology and back-office consolidation. However, the regulator warns that detail in the plans is “variable” and few mention “financial benefits and timescales”.
STPs have come under criticism recently after it emerged that some areas are considering hospital closures.
An investigation by NHE’s sister title PSE then found that health devolution in Manchester has been more successful at delivering integrated care than the STPs.
NHS Improvement and NHS England have now agreed ‘financial control totals’ with individual trusts and CCGs, which represent a minimum level of financial performance that their boards will be held accountable for delivering.
As a result of these measures, providers’ deficits have begun to shrink, but Sally Gainsbury, senior policy analyst at the Nuffield Trust, warned that they could be short-term savings hiding a “more troubling picture”.
Alex Callaghan, deputy head of strategy and policy at the Royal College of Physicians (RCP), has argued that NHS Improvement’s focus on “reducing the pay bill” could have a harmful impact on staffing levels.
The NHS Improvement Board was also asked to approve a single oversight framework which the regulator will now use to oversee providers. It currently uses the risk assessment framework from its predecessor, Monitor, for foundation trusts, and the NHS Trust Development Authority’s accountability framework for trusts.
The framework is based on five themes: quality of care, finance and use of resources, operational performance, strategic change and leadership and improvement capability, and is intended to deliver greater autonomy for trusts.
Responding to the consultation about the framework, 71% of NHS providers and other respondents said they agreed with NHS Improvement’s approach to oversight of providers and 70% said they agreed with its oversight of care quality.
However, just 59% agreed with its approach to overseeing finance and use of resources, 51% agreed with the metrics used to do so, and 34% agreed with the metric weightings.
The latest edition of NHE features in article by Miriam Deakin, head of policy at NHS Providers, on what the single oversight framework will mean for trusts.
Have you got a story to tell? Would you like to become an NHE columnist? If so, click here.