07.10.15
UK has best palliative care in the world – but services still ‘inadequate’ for some
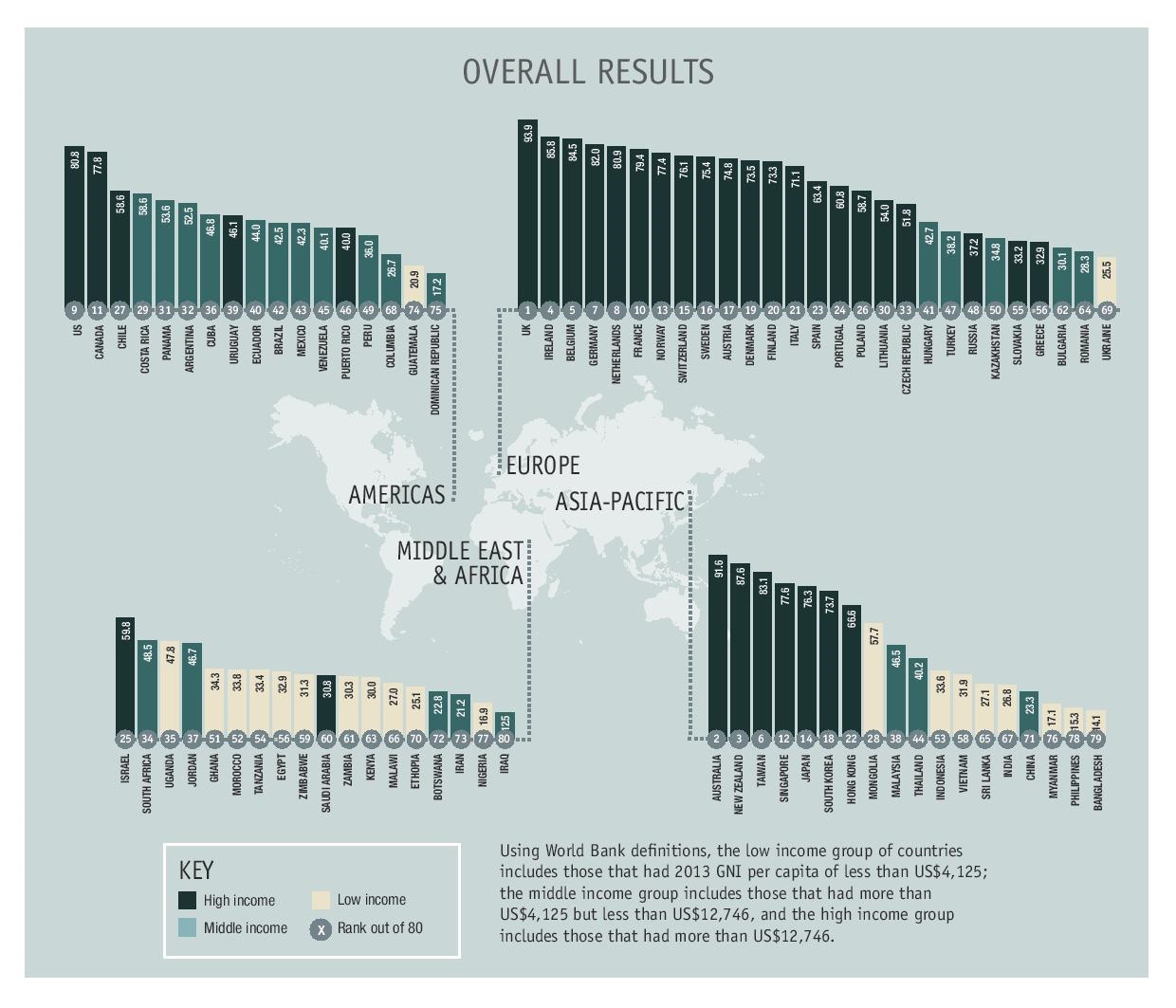
The quality of palliative care offered in the UK has been ranked the best of 80 countries around the world, according to research by the Economist Intelligence Unit (EIU).
Amongst the reasons for this was the existence of “extensive integration of palliative care into the NHS”, as well as comprehensive national policies, a strong hospice movement, and “deep community engagement” on the issue.
The UK also came first in the previous ‘Quality of Death Index’ five years ago.
 Click on the image to enlarge it.
Click on the image to enlarge it.
The index, commissioned by Singaporean philanthropic organisation Lien Foundation, is based on “extensive research” and interviews with more than 120 palliative care experts worldwide.
Annie Pannelay, of EIU healthcare, said: “A very strong marker in our index is the availability of specialised palliative care workers and this is where the UK scores particularly well.
“The UK has a long history of providing treatment in palliative care. The other super strong marker is the way that the countries do have a plan for palliative care. That means they are on the dynamic of measuring progress and improving.”
The report added that the UK’s leading position was explained by both the public and non-profit sectors.
It said: “With a strong hospice movement – much of it supported by charitable funding – palliative and end of life care are both part of a national strategy that is leading to more services being provided in NHS hospitals, as the country works to integrate hospice care more deeply into the healthcare system.”
Despite this, the report noted that the UK is “still not providing adequate services for every citizen”, although it indicates that this “underlines the challenge facing all countries”.
It cited an investigation carried out by the Parliamentary and Health Service Ombudsman in May, which looked at complaints about end of life care in the country. The investigation had highlighted “tragic” cases that illustrated persistent problems, including poor symptom control, poor communication and planning, not responding to the needs of the dying, inadequate out-of-hours services and delays in diagnosis and referrals.
Pannelay added: “There are some concerns, but there is a plan to improve and the single fact that there is a parliamentary report on that and it’s available publicly means a lot – that means the UK is working on it.”
The report also noted that it was “ironic” that countries “struggle to cope with rising healthcare costs” while investing in palliative care could be a more “cost-effective way of managing the needs of an ageing population”.
And Ros Taylor, national director at Hospice UK, said that “significant improvements” could be made in palliative care even without “large investments”.
Taylor, who took part in the report, said: “The things that make a better death are so simple. It’s basic knowledge about good pain control and conversations with people about the things that matter – that could transform many more deaths.”
The study also criticised the chronic underfunding of research into palliative care – a “tiny proportion” of overall healthcare research.
But Public Health England (PHE) and NHS England recently devised a new data collection system set to improve the way adult specialist palliative and end of life care services are recorded. It will implement individual-level data collection nationally to provide a bigger picture of the quality of services nationwide.
The data system, due to roll out in July 2016 and fully implemented by April 2017, was announced shortly after a report prepared for the Scottish Parliament Health Committee found that more than 10,000 Scottish people were dying each year without appropriate palliative care.
Part of this was explained by a “serious information deficit on data available relating to its provision countrywide”.
And in England the situation isn’t any better: Dr Jonathan Koffman, senior lecturer in palliative care at King’s College London, said in September that the care of dying patients was still “inconsistent” and of “poor quality”.