01.02.15
Revolutionising care access for MND patients through telehealth
Source: National Health Executive Jan/Feb 2015
Dr Esther Hobson, National Institute for Health Research doctoral research fellow at the Sheffield Institute for Translational Neurosciences, discusses how a new telehealth and web resource could help revolutionise access to care and support for people suffering from Motor Neurone Disease. David Stevenson reports.
Motor neurone disease (MND) is a rare condition that affects about two in every 100,000 people each year in the UK, with about 5,000 people living with the condition across the country at any one time.
Probably the most famous MND patient is the renowned theoretical physicist Professor Stephen Hawking, who has been battling the severely life-shortening condition for 50 years.
As it progresses, people with MND find activities such as gripping, walking, speaking, swallowing and even breathing increasingly difficult – and eventually impossible.
There are 19 specialist MND Care Centres in the UK, some of which offer support to patients across wide geographic areas. However, for many MND sufferers, travelling to receive care at these sites becomes more difficult – and eventually impossible – as they become more unwell.
While there are no effective treatments for MND, the challenge for doctors and carers is to ensure patients can get access to specialist care and support when they need it.
TiM
A new telehealth system and web resource, developed by experts at the University of Sheffield, could help revolutionise access to care and support for people with the debilitating disease.
The TiM (telehealth in motor neurone disease) system, masterminded by consultant neurologist and MND specialist Dr Chris McDermott, is provided in the form of an app on a tablet device. The app is compatible with Android devices at the moment, but there are ambitions to extend this to Apple.
Through the app, patients are asked to answer questions weekly on their condition and whether they are experiencing mobility issues, cramps, pain or other difficulties. The responses are sent to that patient’s specialist MND care team to swiftly identify any issues and points for action.
TiM is in its infancy and an initial 40-patient trial has just started at the Sheffield MND Care Centre, funded by a National Institute for Health Research (NIHR) fellowship to the trial’s manager, Dr Esther Hobson.
NHE met Dr Hobson at the Sheffield Institute for Translational Neurosciences, where she told us: “The aim of TiM is to improve the communication we have with patients while also giving them a link to the clinic when they can’t get here.
“Some patients have very stable MND and they don’t need to come to clinic, so we can make it a more patient-centred approach.
“When they fill in a question, if their answers change, they get messages and little tips giving them educational information – directing them to certain sites or information on our knowledge centre. We also encourage people to call our MND helpline, which is staffed by a nurse who can provide clinical support for patients and GPs in the area.”
There has been a two-year development of the user-friendly app, and now the three-year trial with patients will help assess how well the telehealth system works for MND patients and their carers.
There has been a lot of support, from patients and charities, for TiM. Dr Hobson is also confident that there won’t be a problem in getting patients signed up for the trial.
Discussing the long-term ambitions for TiM, NHE was told: “This could have big applications in lots of departments. While MND is not a very common disease, a lot of the neurological conditions we see have similar problems –walking, mobility, falling, problems with speech and swallow and symptom management.
“In terms of chronic neurological problems, the applications could be very wide, especially as lots of people now have smartphones or tablets.”
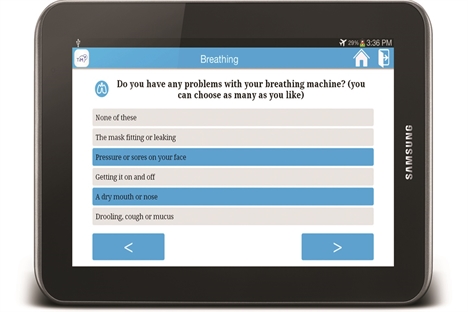
The technology is relatively straightforward to use, and as part of the trial patients get a tablet to use to submit their responses.
TiM hasn’t just been developed with the patient in mind. “We’re involving carers and we have questions for them as well,” said Dr Hobson. “One of the things we do know about MND is that the impact on carers can be huge and, often, they’re providing 24/7 care without any respite. Anything we can do to find out what their experiences are and what the best support can be for them, is potentially huge.”
myNIV
Developed in parallel to TiM, a new web resource has been created to provide essential guidance on the use of vital breathing equipment for people with MND, anywhere in the UK.
Non-invasive ventilation (NIV), which delivers slightly pressurised air into the lungs through a face mask to supplement patients’ own breathing, has been shown to prolong and improve the quality of life for MND sufferers. However, getting to grips with and using NIV can be an obstacle for many patients.
The myNIV web resource, designed by people living with MND and their carers, helps people ‘get to know’ their NIV machine – allowing them to use it with greater ease and confidence.
The portal is the first stage of a project called myMND, which will be joined by other web resources covering key aspects of living with MND, and provides top tips, background information and patient videos on how to use NIV. One video, which looks at ‘bedtime with NIV’, focuses on a couple called Beryl and Dennis who say that “just because the machine is there doesn’t mean the person wearing it has changed”.
Beryl said: “That person still wants the same physical contact. You don’t need to get into bed and immediately put the mask on, it can be that you sit on the bed and do a crossword, or whatever, but then when it is time for bed the mask goes on.”
The web resource came about after a patient study on using NIV. Dr Hobson said: “We found that whenever something changes in MND it signifies progression, and that is difficult for patients and their carers.
“Then, if you give them something like the mask, which is a medical device, it is hard for people and takes a lot of perseverance for people using it. What came out of the research is that we need a better way of educating people about this. I also think this has further applications, such as a site for my wheelchair, feeding tubes etc.”
Joined-up approach
There are aspirations to eventually link the telehealth and web resource together, providing a valuable resource for MND patients across the country.
Dr Hobson said myNIV is a good model for how a patient-driven website, partly supported by clinicians, can help provide support.
“It is reliable information that is well-worded and accessible,” she added.
“My hope is that if you need NIV, although it isn’t all roses, you might come to this website and at least you can explore it, find out more information and see how people are using the technology.”
In the longer term, after the pilot study, the aim is to make the TiM technology widely available to MND patients.
Emily Goodall, whose father suffered from MND, said the app and web resource have the potential to make a huge difference to people with the condition, particularly those living in rural areas where travelling to hospital is very difficult.
“These sorts of things are the way forward, because these are what patients want: accessible information that is reliable, easy to understand and bite-size,” said Dr Hobson.
“I’d very much like the community MND teams to have access to this information, and there is no reason it shouldn’t be provided to GPs as well. You have to be careful, though, that you don’t overload people with information. So, one of the things we’ll be learning is how you flag the right things up at the right time.”
Tell us what you think – have your say below or email [email protected]