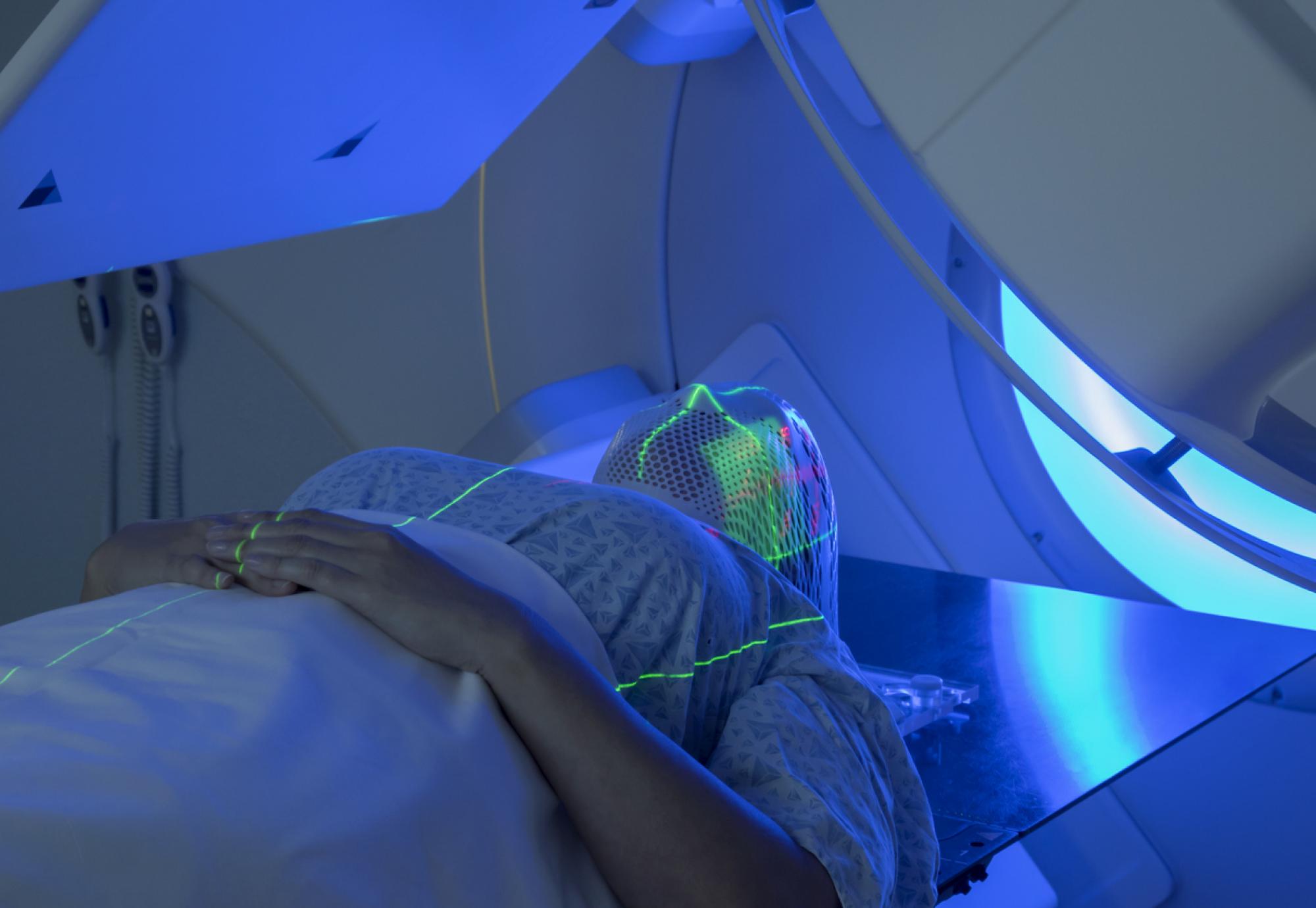
Results from a recent trial have discovered that cancer patients suffered less adverse side effects when treated with dysphagia-optimised intensity modulated radiotherapy (DO-IMRT), rather than just standard IMRT.
The results from the two-year Dysphagia-Aspiration Related Structures (DARS) trial were presented at the American Society for Clinical Oncology at the start of this week and concluded that DO-IMRT could be “practice-changing” for the NHS.
DO-IMRT, which has been developed by researchers at The Royal Marsden NHS Foundation Trust and The Institute of Cancer Research, London, is designed to reduce the risks associated with swallowing difficulties for patients with head and neck cancer.
Some of the swallowing difficulties, or dysphagia as its known in the medical industry, are circumvented by reducing radiation to the pharyngeal muscles, which support swallowing.
The study found that double the number of patients treated using DO-IMRT (40%) reported being able to swallow as normal, compared to those patients being treated with standard IMRT (20%), in the two years following the procedures. Similar results were reported after just one year as well.
Professor Chris Nutting, Consultant Clinical Oncologist at The Royal Marsden NHS Foundation Trust and Professor of Radiation Oncology at The Institute of Cancer Research, London, said: "This practice-changing study represents a major step forward for treating head and neck cancer patients.
“We’ve shown that this optimised IMRT treatment can spare patients’ swallowing muscles and, crucially, without lessening the success of their treatment.
"This new technique, which can have a major impact on patient’s quality of life, is achievable for all centres currently offering IMRT. It simply requires some additional time from the radiation oncologist and physicist to make adjustments to help reduce the irradiation of the muscles that control swallowing. Next, we’re planning to teach others around the world how to reproduce this new treatment approach."
The study also found that more than four in five (81%) people treated with DO-IMRT experienced a high normalcy of diet, meaning they could eat as normal, including foods that required more chewing. The research also found that over nine in ten (92%) people felt comfortable eating in public, compared to just below 73% and 85% for those treated with just standard IMRT respectively.
Approximately 12,400 people are diagnosed each year with head and neck cancer in the UK and around 70% of those experience swallowing difficulties.
Professor Emma Hall, Deputy Director of the Clinical Trials and Statistics Unit at The Institute of Cancer Research, London, said: “Radiation is a vital treatment for patients with head and neck cancer but it can damage important muscles involved in swallowing and talking.
“This cutting-edge radiotherapy technique delivers more precise radiotherapy – targeting cancer cells while sparing these important structures. I am very pleased that the latest results of the DARS trial show the potential of DO-IMRT to reduce side effects from radiotherapy and improve patient’s lives.”
The DARS trial was funded by Cancer Research UK with support from The National Institute for Health and Care Research and The Royal Marsden Cancer Charity.
More information on the DARS trial and its findings is available here.