Private healthcare is not a silver bullet for cutting waiting times, a new study from the Health Foundation has concluded.
The report indicates that, despite the widespread support for independent sector providers (ISPs) within Westminster, the private sector will only have a “limited impact” on tackling things like NHS backlog and cannot solve other issues such as the spate of different workforce-related challenges and general underfunding.
The report zeroes in on the private sector’s role in NHS-funded ophthalmic and orthopaedic care – two areas which have seen the greatest uplift in independent provider activity.
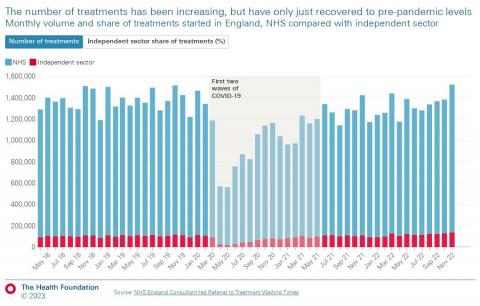
In its first instance, the report draws attention to the fact that the overall number of NHS-funded treatments has only just recovered to pre-pandemic levels, with ISPs being responsible for 8.7% of the care – a 1% increase from before COVID-19.
The study also found that ISPs have greatly increased the number of inpatient ophthalmic care procedures they perform on behalf of the health service, with data indicating that nearly four in 10 (38.6%) procedures were carried out by ISPs in February 2022. This is a jump from just over two in 10 (23.3%) pre-pandemic.
Similarly, ISPs delivered almost a third (31.2%) of inpatient orthopaedic care for the NHS in February 2022; an increase from around a quarter (26.8%) before the pandemic.
The Health Foundation say the smaller jump is because the increase in ophthalmic care is primarily down to cataract procedures, which make up 60-70% of all ophthalmic care and are easily scaled up – something that is not being reflected in most other areas of ophthalmology or orthopaedic care.
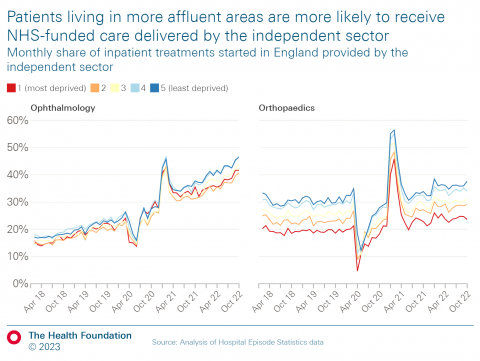
The new report also shone a spotlight on some of the inequalities observable when accessing private healthcare, with the Health Foundation’s analysis showing that the amount of treatment being delivered in the most deprived areas is still 1% lower than pre-pandemic levels.
Conversely, treatment volumes in the most affluent areas were 5% higher – the Health Foundation put this down to the increased likelihood of ISPs being located in richer areas.
White patients are also more likely to receive ISP-delivered NHS care compared to patients from other ethnic groups across both specialties, according to the Health Foundation’s report.
The Health Foundation’s director of data analytics, Charles Tallack, said: “Patients are facing unacceptable waits, and the NHS has a huge challenge to increase activity to the levels needed to bring down waiting lists.
“Our study shows that, while it has an important role to play, the independent sector is not a panacea for bringing down waiting lists, despite it being at the heart of the elective recovery plan.
“To truly increase activity and bring down waiting lists, the government must address the major problems facing the NHS – from the lack of an adequate workforce plan to historic under-investment, as well as pressures in social care.”



















