The NHS’s Getting It Right First Time (GIRFT) team—in partnership with the Royal College of Physicians (RCP)—have published new guidance to help improve patient flow and experience within urgent and emergency care.
Using the document, the RCP has said that operational teams can work with clinicians to:
- benchmark whether their service is delivering the requisite care and inter-specialty working;
- identify any gaps or shortcomings; and
- collaborate with colleagues and executives to ensure the principles are supported and applied.
“We know that delivering acute care for medical patients needs joint working of specialties,” said Dr John Dean, who is the RCP’s clinical vice president and the lead on the work with the GIRFT initiative. “These principles bring together much previous guidance into a single place. Local clinical leaders across specialties should work with operational colleagues using these principles to enable the care delivery they want to provide.”
The principles are backed up by an overarching theme—that patients should have equitable access to professionals with the skills required for their care, independent of the location of their bed or the nominal admitting specialty.
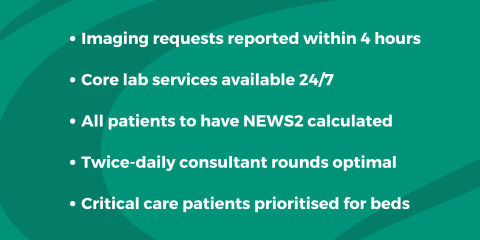
The principles include that all urgent cross sectional (CT/MRI) imaging request should be reported within four hours. Core laboratory services should be available 24/7, and turnaround times should be regularly monitored with reports coming on a monthly basis. The third one is that every patient should have NEWS2 calculated, which should be used in conjunction with the patient’s presenting condition to prioritise care.
All patients should also have a full assessment undertaken by a competent clinical decision maker—ideally within one hour and within a maximum of four hours of the decision to admit/arrival on assessment unit. The document defines competent clinical decision makers as those who can perform an initial assessment and treatment of a patient.
The fifth principles centres around every patient being reviewed by an expert clinical decision maker within six hours of the decision to admit/arrival on assessment unit. An expert clinical decision maker is defined as those who can develop comprehensive management plans and have overall responsibility for patient care while having extensive experience in managing acute patients within their specialty.
Upon agreement that a patient should be transferred from the assessment unit to a non-medical ward, the receiving specialty team becomes responsible for the patient makes up the sixth principle. The seventh is that those being transferred out of critical care units should be prioritised for inpatient bed allocation. Number eight is that where specialties provide an admissions unit, an expert/senior decision maker should receive referrals and provide advice to the community and hospitals every day to prevent unnecessary hospital attendance/admission and to facilitate hospital discharge.
A senior decision maker is defined as those who can collate relevant patient information, make a diagnosis and determine a management plan.
Twice-daily consultant ward rounds is the optimal model and should be delivered in higher acuity areas, and other medical wards if possible, according to the RCP’s guidance. The 10th and final principle is that patients who are over 65 should be assessed on arrival using the clinical frailty scale and 4AT tool for delirium.
Image credit: iStock



















