Results from a new study have revealed that the two-year survival rates for head and neck cancer patients following transoral robotic surgery (TORS) are significantly better than for other treatments.
The RECUT study, which was funded by The Royal Marsden Cancer Charity and the Oracle Cancer Trust, analysed 278 different cases of recurrent head and neck cancer from 16 sites across three continents.
The research found that the overall survival rate for patients who had their recurrence identified at an early stage was almost three in every four (72%), which is ultimately better than the alternative treatment options for this patient group, which includes open surgery, radiotherapy, chemotherapy, and immunotherapy.
Previous research has reported that the two-year survival rates for patients treated with intensity modulated radiotherapy (IMRT) were approximately 40-50%, whilst the rates for those treated with IMRT as well as open surgery were just 62%. The figures for open surgery alone were 52%.
The report also found that TORS can offer cancer patients a significantly better quality of life compared to other treatments – RECUT revealed that, after TORS, approximately two-fifths (38%) of patients needed a tracheostomy to support their breathing and 39% needed a gastrostomy for eating. After just a year though, these figures dropped to just 11% needing a tracheostomy and 34% still requiring a gastronomy.
Most importantly though, 74% of patients were able to eat soft foods or more.
Comparatively, previous studies investigating similar things, but for open surgery, have indicated that following the procedure, around four-fifths (79%) of individuals needed a tracheostomy and three quarters (75%) needed a gastronomy.
Study Lead Professor Vinidh Paleri, who is a Consultant Head and Neck Surgeon at The Royal Marden NHS Foundation Trust, said: “These exciting results demonstrate that TORS, a cutting-edge robotic surgical procedure, offers durable survival for patients with recurrent head and neck cancer compared with current standard treatments, such as open surgery.
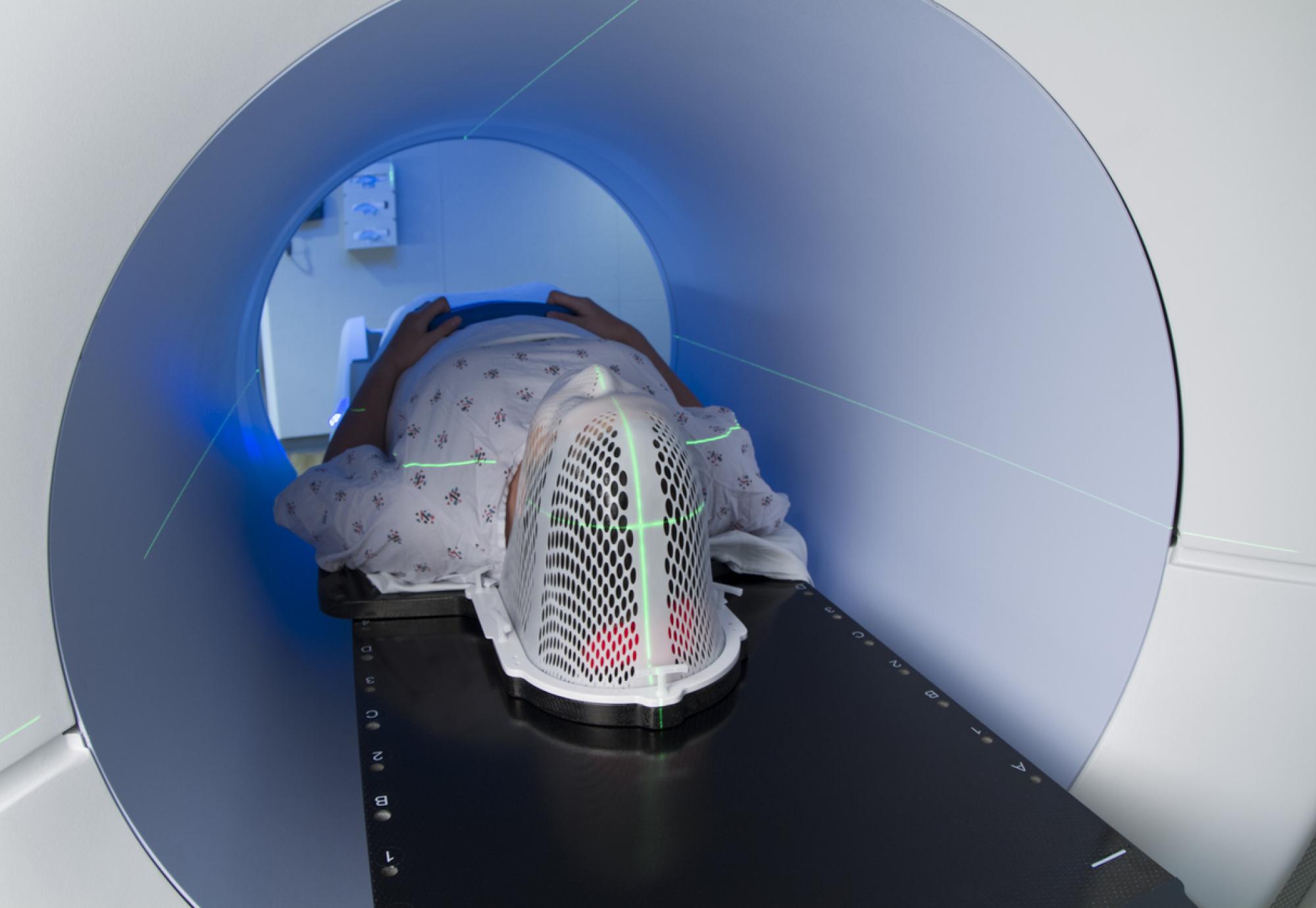
“Until now, there was little evidence that robotic surgery could improve outcomes for patients with this disease. Recurrent head and neck cancer can be incredibly difficult to manage as patients have already been treated, often with surgery and radiotherapy, which can cause anatomical changes, scarring, and impaired healing. For these patients, the very latest in surgical technology and treatment is vital for successful treatment, so TORS is an extremely welcome innovation.
“Crucially, this study also suggests that TORS can improve the quality of life of people with the disease. Treatment for recurrent head and neck cancer can have a devastating impact on the ability to speak and eat, which are so fundamental to our enjoyment of life, and this minimally invasive technique can offer patients faster recovery times, with reduced need for medical equipment to support breathing and eating.”
After his oropharyngeal cancer came back in 2019, Professor Michael Thick, 71, from Norfolk went back to The Royal Marsden to be treated using robotic surgery.
Today, Michael is cancer-free.
He said: “As a former transplant surgeon, I know a fair bit about cancer and its treatment and, while I hoped I had been cured in 2009, I knew there was a chance it would come back. In 2019, when I noticed swallowing felt uncomfortable and slightly painful, I mentioned my concerns to my consultant who, after tests, confirmed the cancer had recurred.
“The treatment following my first diagnosis left me a fraction of my original weight and extremely unwell. My recovery was slow, and it took over a year to return to work. Fortunately, in 2019, I was offered robotic surgery to remove the cancer. It was a very attractive choice as the alternative would have been very unpleasant; open surgery where my jaw would have been split, followed by full facial reconstruction.
“After the operation, I was able to go home after just three nights in hospital and my recovery was thankfully quick and uneventful. The surgery was a success, and I’m now cancer-free. I’m also able work, pursue my hobbies – from beekeeping and deer management, to flying planes and sailing boats - and I can speak and eat with care.
“Without The Royal Marsden combining leading-edge research with clinical practice, I wouldn’t be here today. When I was first diagnosed, I was treated through a clinical trial and the second time, I was offered robotic surgery, an innovative new option for recurrent head and neck cancer patients at the time. Thanks to them, I’ve returned to normality.”
TORS is type of robotic surgery pioneered by health professionals at The Royal Marsden NHS Foundation Trust.