Clinicians across the country are working tirelessly to respond to the unprecedented pressures currently facing the NHS. We hear, read and live this first-hand every single day. To help tackle a waiting list currently standing at more than 7.5 million patients,[1] it is crucial that we harness technology to support both better patient outcomes and sustainable productivity improvements for the health and care system.
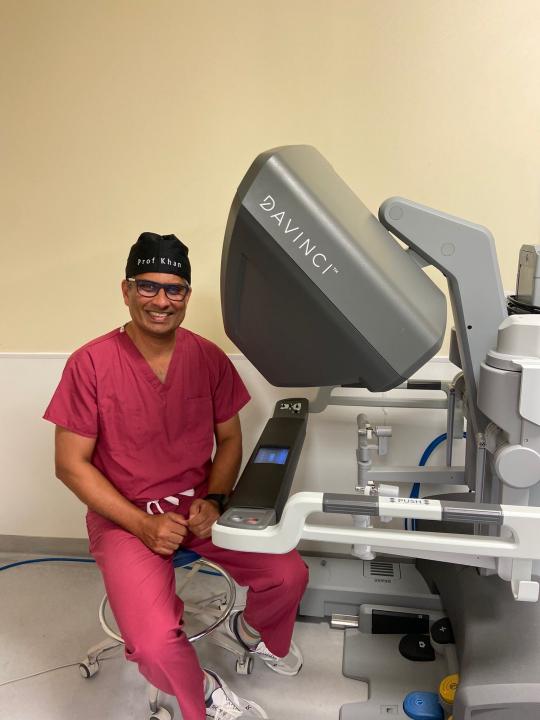
I’ve been a consultant surgeon in Portsmouth for nearly 16 years. During this time, few technological advancements have been as transformative for our work than robotic-assisted surgery (RAS).
Watching our RAS programme evolve and seeing the impact this has had on patients has been extraordinary. We introduced our first da Vinci system in our main theatres, initially for cancer procedures, and then expanded to five additional clinical specialties. Most recently, we were delighted to launch the UK’s first-ever robotic-assisted day case surgery programme, where we’ve been able to perform more than 400 day case surgeries on a dedicated syste
The benefits of our approach are clear: my own data shows that patients who undergo RAS spend fewer days in hospital, experience fewer complications, and are half as likely to require a readmission to hospital when compared with laparoscopic surgery.[2] We have shown that there has been a significant improvement in overall survival for cancer patients at five years with the use of RAS in our cohort.[3]
Supporting the wider uptake of this technology across the NHS would likely offer improved patient care, in turn enabling a productivity boost to hospitals across the country responding to rising patient demand.
Delivering cost-efficiencies
Strengthening productivity is not the only goal. We also need to show how a successful RAS programme can bring economic benefits to the NHS. RAS is in fact proved to be better - we’ve estimated that there is a potential downstream cost avoidance of more than £1,000 per patient, if certain procedures are performed as RAS rather than laparoscopically. [4] This is a direct consequence of improved patient outcomes, but also the impact that our programme has had on utilising healthcare resources effectively.
Increasing productivity and staffing efficiencies
The evolution of our robotics programme has helped us to treat more patients and optimise our hospital processes. The da Vinci system streamlines workflow and provides greater surgeon autonomy, the team’s time can be repurposed to help other operating teams whilst the surgeon is mid-operation – helping to improve flow throughout our hospitals and ultimately treat more patients. During certain procedures in my robotic theatre, this has enabled us to safely perform procedures with up to two fewer team members compared to a laparoscopic approach.[5]
Futureproofing the next generation
I’m particularly excited about the opportunities that robotic technology can provide for the next generation of surgeons across the country. By using a standardised training programme for surgical trainees, we can inspire and equip them with the skills needed to meet future healthcare needs.
Introducing the dual console da Vinci Xi system to our hospital’s Day Surgery Unit has had a significant impact on opportunities for our trainees to develop as a bedside or as a console surgeon. The second surgical console enables them to gain valuable experience by performing simpler procedures with the support of our consultants, in preparation for training in more complex cases.
We recognise that our NHS is under a lot of pressure. However, through the empowerment of clinicians and care teams across the country we can utilise technology to deliver improved patient care, boost productivity, and crucially lower the total cost to treat per patient episode.



















