09.04.15
A new financial year for the NHS but not a new beginning
Guest blog by Phillippa Hentsch, chief policy advisor for funding and resources at NHS Providers, who looks at the financial landscape facing providers in the next 12 months.
Where are NHS finances now?
As highlighted by the King’s Fund last month, the NHS has been required to absorb the shock of moving from 14 years of average real term increases of 5.6% to the past four years of 0.8%.[1] Although the NHS has coped well with this squeeze during the first three years of the parliament, and we would argue continues to perform exceptionally well given the scale of the challenge, there can be no denying that there is now a financial crisis in the NHS.
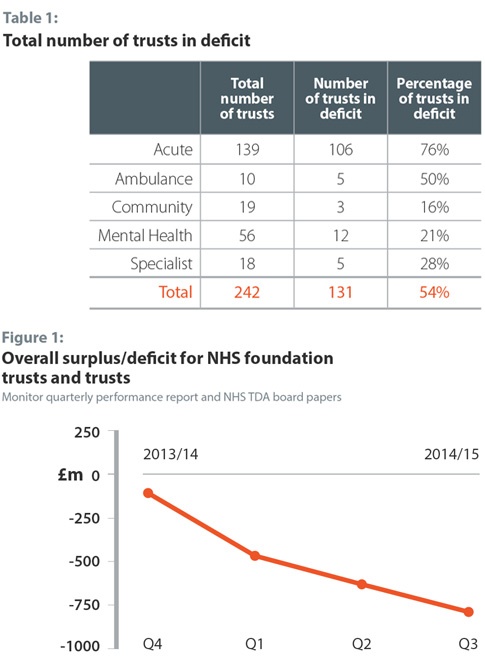
The problems are now so widespread – not just in the number of foundation trusts and NHS trusts currently in deficit[2] (table 1), but also by the increasing size of provider deficits (figure 1) – that no part of the provider sector is immune and even large international teaching hospitals with a diverse range of services and income are starting to raise red flags.
What is 2015/16 looking like?
As we start the new financial year, the outlook for 2015/16 is not positive. Compared to this time last year, there are more providers in financial distress; more requiring additional financial support[3],[4]; more struggling to contain temporary and agency spend – last week I learnt of one NHS trust where agency spend was up 131% year on year – and an increasing number of finance directors concerned about their ability to meet their cost improvement targets.[5] This is hardly the solid base necessary for the NHS to weather the financial storm of 2015/16, which has been described by us and others as the most challenging year in recent NHS history.
Against this backdrop, the annual national tariff and contracting round has been playing out, which has been described by many as the most bruising ever experienced. Although the new proposals put forward by NHS England and Monitor last month largely resolved the impasse with the national tariff at the national level (well at least for all apart from some of the largest hospitals in England, which provide almost 40% of all NHS services, who rejected both options put on the table).
The vast majority of providers who picked the enhanced tariff option (ETO) didn’t do so because they thought it was a realistically deliverable package; unfortunately they chose it as the least worst option, only marginally better than the original proposals in the statutory consultation or the default tariff roll over (DTR), which would have cost them the 2.5% in income they currently have the possibility of earning back through Commissioning for Quality and Innovation (CQUIN) payments.
When we asked finance directors how confident they were in the financial sustainability of their trust in 2015/16 under the different tariff options, only 15% of NHS providers were confident under the ETO, compared to 13% under the proposals in the original statutory consultation and 3% under the DTR.[6] This is hardly a glowing endorsement of the ETO, which the majority of providers are now required to cope with for 2015/16, and also suggests that for trusts listed on the DTR this wasn’t necessarily a positive affirmation of the rollover approach but rather the consequence of not choosing either option.
In saying this, I don’t underestimate the scale of the challenge which faced NHS England and Monitor in putting together the tariff 2015/16, it was an almost impossible task but one which certainly could have been managed differently. There is now unfortunately a gulf between the centre and local NHS organisations, and bridges will have to be built when setting the 2016/17 tariff if we are to avoid the mistakes from this year. The objection to this year’s tariff was a warning from the NHS provider sector that continuing to drive an unsustainable level of efficiency through the payment system is no longer safe – unless this changes, no doubt the objections will keep coming.
The added challenge for 2015/16 is that although the impasse might have been resolved at the national level, it has not been resolved at the local level, with many provider and commissioner contracting teams still far apart as we enter the new financial year. Just to cite a couple of examples, we are hearing of:
- Commissioners unable to afford the ETO;
- Providers who opted for the ETO being asked to deliver undeliverable CQUINs (despite this clearly being one of the key advantages of choosing the ETO);
- Providers and commissioners heading in to arbitration when they agree on activity plans, but disagree on how to afford them;
- Only a handful of commissioners (CCGs and local area teams) increasing their real term investment in mental health services in line with the planning guidance;
- Schemes previously funded from the marginal rate for emergency admissions, such as community services, admission avoidance initiatives and resilience funding, are being reduced or cut. The change in the marginal rate was supposed to be about unlocking more not less investment for urgent and emergency care;
- Providers of specialised services unsure how to fund care under the new marginal rate without compromising patient safety, or divesting themselves of specialised service lines which will in turn have implications on staff and other services provided.
This all means that this year’s contracting round has been and continues to be particularly challenging – only 7% of our members thought that the majority of their 2015/16 contracts with commissioners would be signed by the start of the financial year[7], with many of our members reporting that they haven’t even received contract offers yet.
What do we need to do?
As we start the new financial year, the NHS is unfortunately not on a firm footing financially, with the provider sector planning to end this financial year over £850 million in deficit, and next financial year between £2-2.5 billion in deficit. NHS providers will continue to prioritise patient safety and quality over financial sustainability but we are coming to a point at which the two principles are intrinsically linked – a Board might be able to make a decision to maintain its investment in staffing by continuing to go further in to deficit, but at the same time, being in deficit will mean limited resources to invest and transform for the future.
Some have suggested that financial deficits have become a new and accepted normal for the NHS, and that Boards no longer get exercised when their finance director reports a financial deficit, as they are now so widespread across the sector. But, this couldn’t be further from the truth – financial stewardship is deeply ingrained in the NHS and when long-standing and experienced finance directors are putting in their first deficit plans in 15 years, this is a symptom of systemic, deep seated problems rather than a new cultural shift towards accepting and tolerating financial failure.
Boards recognise that quality and finance are intrinsically linked and that an inability to invest in services today will have implications for patient services tomorrow. The past five years have forced the NHS to lurch from one quick fix to the next to try and contain the looming financial crisis but this strategy will not get us through the next five years. The new government, together with the national bodies, need to heed the warning and work with the sector to come up with a realistic and deliverable set of proposals to support the NHS meet its funding challenge in a stable, more transparent and sustainable way.
[1] http://www.kingsfund.org.uk/publications/nhs-performance-under-coalition-government
[2] Please note that our classification of acute, ambulance, community, mental health and specialist trusts might slightly differ from other sources.
[3] http://www.hsj.co.uk/news/finance/exclusive-dh-bailouts-already-higher-than-2013-14-total/5081970.article#.VRksxOH2RkU
[4] http://www.hsj.co.uk/news/finance/exclusive-dh-agreed-extra-bailouts-for-trusts-where-performance-was-at-risk/5083337.article#.VRkgWuH2RkV
[5] http://qmr.kingsfund.org.uk/2015/14/survey
[6] NHS Providers survey, March 2015. Sample size = 38 finance directors from NHS trusts and FTs
[7] NHS Providers survey, February 2015. Sample size = 43 finance directors from NHS trusts and FTs
Tell us what you think – have your say below, or email us directly at [email protected]