21.06.17
Using demand and capacity modelling to deliver quality care
Ricky McCullough, deputy head of performance at Royal Free London NHS FT, tells NHE about using demand and capacity modelling to deliver quality care to patients and meet national waiting list targets.
At a time when hospital budgets are stretched, and with an increased focus on meeting government waiting list and waiting time targets, managing demand and capacity within the NHS has never been more important.
The mismatch between, and variation in, capacity and demand is one of the main reasons why waiting lists or backlogs develop and waiting lists and waiting times increase within NHS services.
At the Royal Free London NHS FT, its deputy head of performance, Ricky McCullough, has been using what he has learnt through the NHS’s National Demand and Capacity Programme to work with colleagues to use demand and capacity planning tools, to improve patient care and meet government waiting list targets.
“Consistently delivering high-quality care to our patients is at the heart of what we do at the Royal Free London NHS FT. Having a robust demand and capacity framework is essential for meeting our performance standards, managing variation in demand and planning for service growth,” said McCullough.
McCullough has already used the pilot training and advice from the Demand and Capacity Programme to support service improvements in two areas: the skin cancer and endoscopy diagnostic clinics.
Meeting the two-week wait cancer performance standard
“Seeing a patient within two weeks of their suspected cancer referral is critical in ensuring that patients get treatment within 62 days should they subsequently be diagnosed with cancer,” said McCullough. “We need to ensure we consistently deliver enough ‘core capacity’- that’s recurrent, job planned capacity that we can rely on - to continue to see our patients within 14 days of their referral.”
To help achieve this, the Royal Free decided to use NHS IMAS demand and capacity modelling tools for all its cancer two week wait (WW) services, starting with skin cancer.
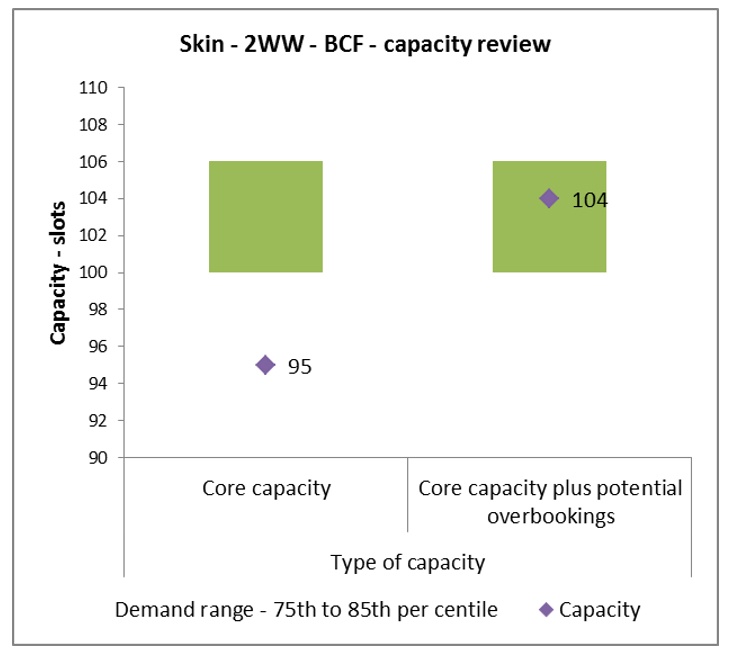
The skin cancer team planned to undertake a complete demand and capacity review to ensure they had the right amount of core capacity to see their suspected cancer patients within 14 days of referral. Due to the large volume of referrals, the skin team was having to put on a significant amount of additional ad-hoc clinic capacity to ensure they were seeing patients within 14 days of referral.
McCullough said: “Arranging additional clinics is a very time-consuming process. Clinical time needs to be secured, clinic space needs to be arranged, clinic templates have to be built and patients contacted. Many of these clinics have to be arranged at additional cost to the service, as they sit outside of existing clinical job plans. This process can be very pressured and stressful.’”
The skin team worked with McCullough and, using the tools and methodology outlined in the NHS’s National Demand and Capacity Programme, measured their demand (and the variation in their demand) over the course of 52 weeks to outline the weekly core capacity needed to deliver the service.
“Nationally, there is a 14-day target for patients being referred to hospital by their GP with suspected cancer,” noted McCullough. “However, we have an aspiration internally to see those patients within seven days – the modelling tools provided by NHS’s National Demand and Capacity Programme supports this.”
Endoscopy
Taking into account national research entitled ‘Scoping the Future’, produced by Cancer Research UK, the Royal Free knows the national picture shows an expected 6.5% growth year on year for GI Endoscopy between now and 2020.
As a result, its endoscopy service has incorporated the demand and capacity work into the business as usual processes for waiting list management. This includes short-term ad-hoc capacity planning, modelling the impact of list closures on the waiting list and optimising endoscopy utilisation, e.g. the rate of patients that did not attend appointments.
In addition, the model has informed business planning. This includes the development of the new endoscopy unit at Chase Farm Hospital and future planning for the endoscopy service at the Royal Free Hospital.
Meeting national standards for waiting lists
When reviewing demand and capacity for a service or function, the first question the Royal Free tries to answer is, ‘are there enough slots being provided on a weekly basis for the demand the service is being asked to provide?’ Firstly, it needs to perform the ‘demand calculation’, which is expressed as follows:
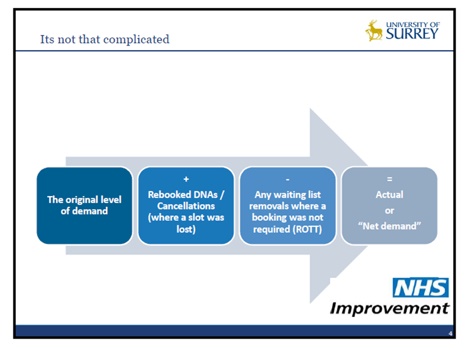
The IMAS methodology suggests setting the capacity needed at the 65th – 85th per centile of the variation in demand; setting capacity between these levels can be thought of as saying ‘we will have enough capacity to see all of our patients around 65 – 85% of the time’.
McCullough said: “If capacity is set at the mean (average), all patients will get seen across the year but waiting times will vary and some patients will experience a long wait.
“We also look at how much of the capacity provided is ‘core’, meaning recurrent, job planned capacity, which can be relied on to continue, versus how much additional ‘ad-hoc’ capacity may be required to meet a performance standard or react to variation in demand.
“If the service consistently needs additional capacity, we will explore the option of converting this additional activity (or a portion of it) into core capacity, which we can rely on to recur consistently. The IMAS methodology suggests setting the weekly capacity at the 65th per centile of the variation in demand as a minimum, though this may need to be higher depending on volume and variation.
“We work very closely with operational and clinical teams to work through the data driving the model to answer the question “does the service have enough capacity on a weekly basis to consistently meet demand? And then, “does the service have enough ‘core’ capacity to meet demand?”
Rolling out demand and capacity training at the Royal Free
In conjunction with the modelling effort, the Royal Free is rolling out a broader demand and capacity training programme tackling the core concepts which drive demand and capacity modelling:
- Definitions of capacity and demand
- Different types of demand for a service
- Accounting for variation in demand
- ‘Ideal’ waiting list sizes
It has developed much of this programme based on work from the national Demand and Capacity Programme ‘Train the trainer’ sessions.
McCullough said: “We aim this training at administrative, operational and clinical members of staff – because they are the people who deliver the services at the clinics and diagnostic centres, develop the job plans for clinicians and manage the waiting lists.
“Our aim is to develop a robust framework to understand, engage with and deliver effective demand and capacity management and planning at the Royal Free – supporting waiting list management, service and job planning.”
Getting buy-in
“It’s not just about getting buy-in from operational staff that’s important. We have buy-in from all tiers of staff to do this; clinicians, operational managers, the Group head of performance up to the executive team and chief executive,” he noted.
The hospital also has a broader demand and capacity group which helps oversee planning across the trust.
NHS Demand and Capacity Trainer Programme
This month sees the launch of a new six-month Demand and Capacity Trainer Programme, as part of the launch of the NHS Demand and Capacity Programme 2017-19, that aims to create a pool of 300-400 trainers over the next three years. Embedded in local health economies, they will be trained to cascade training and support on demand and capacity planning modelling within their organisations.
Ricky said: “I’ve already done a couple of sessions with the National Demand and Capacity Programme; a three-day training course in Surrey University and a one day session in London.
“I found it very helpful – not only did they go through best practice in terms of using the demand and capacity tools, but we also spent time discussing and rehearsing the methodology itself, and how it could be practically applied in the operational environment.
“Further to this, we participated in a series of practical exercises to put our learning to the test – we were given dummy data sets and instructed to run the numbers through the demand and capacity tools.
“At the end, we did a feedback session outlining what we thought the challenges were. Generally, these were: understanding your demand; shaping your capacity to meet that demand; and the fundamental importance of accounting for variation in demand.”
Service benefits
Securing additional appointments within core capacity is likely to be cheaper than outsourcing, or using Waiting List Initiative funding. Traditionally, the trust has reacted to increases in demand by putting on more core (or additional) clinics on top of existing provision, but increasingly it is thinking about delivering services differently, and using finite resources as effectively as possible. The demand and capacity modelling has supported this:
- Where additional capacity is required, the demand and capacity tools can be used as part of a structured approach to identify where the bottlenecks are, and suggest the weekly number of slots needed improve patient flow.
- The trust’s demand and capacity modelling has focused its attention on specific parts of the clinical pathway, such as the ‘straight to test’ (STT) diagnostic element. As part of a STT pathway it performs clinical triage on each 2WW referral to understand if it is appropriate for the patient to be seen directly by the diagnostic team. This may result in it saving a clinic slot to be used for a patient who does need a 2WW consultation as part of their pathway.
Patient benefits
Robust demand and capacity management can improve the patient experience in the following ways:
- Patient choice – when demand and capacity are in balance, you can expect patients to have choice as to which appointment time and date are convenient for them
- Patient experience – when capacity meets demand, you can expect less need for patients being overbooked into clinic, resulting in more time with the clinician and better clinic experience overall
- Patient wait – setting capacity in line with demand results in less need for additional clinics (which can be time-consuming to set up), and will likely result in a shorter wait time for the patient.