23.12.15
New NHS planning regime shows 'fundamental change of direction'
All NHS organisations in England must develop two “separate but connected” plans early next year as part of the planning guidance for 2016-17 to 2020-21 – detailing the strategies for their local health and care system and within their own organisation.
The two plans will be split into a five-year ‘sustainability and transformation plan’ (STP), which will be place-based and focus on driving the FYFV; and a one-year operational plan for 2016-17, which will be organisation-based but consistent with the emerging STP.
In the planning guidance, NHS leading bodies said the scale of what is needed in the future depends on how well organisations end the current year – reiterating what NHS Improvement’s Jim Mackey had already revealed.
“The 2016-17 financial challenge for each trust will be contingent upon its end-of-year financial outturn, and the winter period calls for a relentless focus on maintaining standards in emergency care,” the guidance read.
“It is also the case that local NHS systems will only become sustainable if they accelerate their work on prevention and care design. We don’t have the luxury of waiting until perfect plans are completed. So we ask local systems, early in the new year, to go faster on transformation in a few priority areas, as a way of building momentum.”
Commenting on the guidance, NHS Confederation’s chief executive, Rob Webster, said: “The spirit of this guidance signals a fundamental change of direction to the way the health and care sector operates. The era of focusing on organisations and their specific regulator is over.
“The move to place-based planning with a focus on collaboration and joined-up services will be a challenge to the national bodies and the NHS – one that we must embrace for the benefit of the people we serve.
“If we are to succeed, we must ensure that NHS England, NHS Improvement and other arm’s-length bodies strike a new deal with local organisations. We must see a careful and consistent balance between tight performance management that potentially crowds out local leadership and allowing local organisations the space and flexibility they need to drive strategic, truly transformational change.”
Webster added that, in the coming months, the NHS Confederation will work to ensure “a clear narrative emerges” to elucidate how this guidance, financial allocations and the Department of Health’s mandate “add up to a coherent framework”.
“In doing so, the legitimate question of local government alignment plans and the means of bridging social care and public health funding must be resolved,” he concluded.
Sustainability and transformation plans
Every health and care system will have to come together to create an “ambitious local blueprint” to speed up the implementation of the FYFV.
These plans will cover the period between October next year and March 2021. They will be subject to a formal assessment in July next year following submission in June.
“We are asking the NHS to spend the next six months delivering core access, quality and financial standards while planning properly for the next five years,” the guidance read.
Place-based planning is based on the idea that the NHS should no longer emphasise an organisational separation and autonomy “that doesn’t make sense to staff or patients”. It will go beyond “just writing a document” and cannot be outsourced or delegated; instead, it will involve strong system leadership.
The five pillars of the STP will be local leaders coming together as a team; developing a shared vision with the local community, involving local government as appropriate; programming a coherent set of activities; executing against plan; and learning and adapting.
Where “collaborative and capable leadership” can’t be established, NHS England and NHS Improvement will “help secure remedies” through joined-up and effective system oversight.
STPs must cover all areas of CCG and NHS England-commissioned activity, including specialised services, where the planning will be led from the 10 collaborative commissioning hubs, and primary medical care. It must be done from a local CCG perspective, “irrespective of delegation arrangements”.
They must also ensure better integration with council services, including prevention and social care.
These place-based plans will become “the single application and approval process” for gaining access to transformational funding for 2017-18 onwards.
Areas with the “most compelling and credible” plans will secure the earlier extra funding from April 2017.
Operational plans
Local system leaders will be tasked early on to run a “shared and open-book” operational planning process for 2016-17 – covering activity, capacity, finance and deliverables from the emerging STP for the next financial year.
Commissioner and provider plans must be agreed by NHS England and NHS Improvement by April 2017, based on local contracts that must be signed by March 2016.
All operational plans must demonstrate how providers “intend to reconcile finance with activity”, with clear plans to balance the books if they have a deficit.
They must outline their plans to deliver the ‘key must-dos’ from an overarching list of nine essential ‘must-dos’, as well as their planned contribution to efficiency savings.
Risks embedded in the local health economy plans must be jointly identified and mitigated through an agreed contingency plan, and organisations will be asked to show how they link with and support the local emerging STPs.
The operational plan should be regarded as ‘year one’ of the five-year STP, meaning NHS England and NHS Improvement expect “significant progress on transformation” through it.
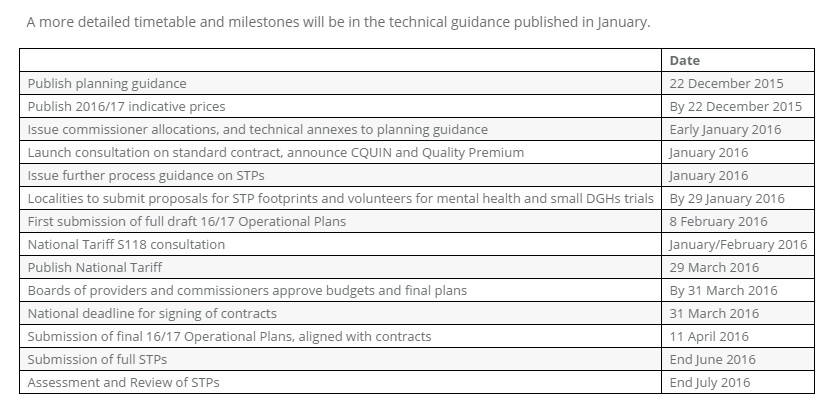
Provided by NHS Confederation, below is a detailed timetable for the upcoming milestones organisations must reach (click to enlarge):
Chris Hopson, chief executive of NHS Providers, noted that the guidance also included the “welcome announcements” of a net 1.1% increase to the 2016-17 tariff (the price paid to NHS providers) compared to last year’s reduction of 1.9%.
He also referred to the £1.8bn ‘sustainability fund’ designed to help providers turn this year’s projected £2.5bn funding gap into a surplus, as well as “recognition that local health and care systems need three year plans to create a sustainable future”.
“This turns a previously impossible looking 2016-17 task into one that looks just about deliverable, albeit extremely challenging,” he said.
“But this extra early investment is only temporary and comes with conditions attached. Trusts and foundation trusts will have a year to turn around their finances, develop long term efficiency savings plans and identify the long term changes their local health and care system need. All this must be delivered whilst continuing to deliver outstanding care to a million patients every 36 hours.
“The pragmatism of today’s guidance and November’s Spending Review settlement are important steps forward. However there are still major hurdles to overcome: finding solutions to longer term problems such as increasing the proportion of GDP we invest in healthcare; ensuring rapid and widespread development of new and integrated care models; and delivering the move to seven day services.”