07.01.16
Groundhog day
Source: NHE Jan/Feb 16
Richard Jones, partner at Moorhouse, says A&E departments act as the barometer for local health economies.
It’s not saying anything new to observe that winter is the busiest time of year for the NHS; the sharp rise in the demand for both primary and acute care puts great strain on the system. In winters past, additional investment has helped hospitals to cope and, whilst not a perfect solution, it enabled the system to manage the peaks of pressure. However, it is now increasingly recognised that short-term investment cannot be the only response to these predictable seasonal challenges.
Over recent years, we have seen consistent year-on-year rises in the scale of the challenge faced by health systems due in large part to a perfect storm of staffing challenges, demand and capacity imbalances, poor flow and local factors. The negative impact on the NHS’s ability to deliver during the cold and dark months seems to be steadily increasing.
Not just winter
Indeed, these challenges can now fairly be described as extending beyond winter: in 2014-15, the NHS failed to achieve the ‘95% A&E All Type’ standard for the year in aggregate for the first time since the standard was introduced. And 2015-16 saw the standard already breached in Q1 and Q2, resulting in an extremely challenging starting point to have entered the winter.
With delivery through summer now also challenged (it’s too early to predict this will be the new normal, but a worrying trend does seem to be developing), whatever breathing space the system may once have had appears to be disappearing. Unless something gives, achieving the A&E All Type standard for winter 2016-17 will be more difficult still. Just as, according to folklore, a groundhog seeing a shadow upon emerging from its burrow heralds six more weeks of winter, so a challenging summer for the NHS predicts a harsher, longer seasonal decline in performance results.
Systemic pressures
A&E departments act as the barometer for local health economies. Failure to achieve the four-hour standard is unlikely to be due to factors solely within the A&E department, but reflects systemic pressures across the hospital and related community services – both upstream (e.g. primary care, 111) and downstream (e.g. community and social care).
The question then is: how can the cycle be broken? There is a clear need to fundamentally redesign the approach to planning for winter, ensuring year-round, system-wide resilience. It’s too late for 2015-16, but what can local health economies do now to start planning for next winter?
Clearly, there’s no simple answer to that question, or we’d have seen a solution by now. But while there may not be a magic pill, our experience suggests there are a number of positive steps health economies can take to deliver sustained performance improvement. Key to initiating any of these is the ability to step back and adopt a wider view of the system as a whole. By contrast, the traditional focus on individual organisations – attempting to fix things solely in the hospital itself – represents a thankless and likely ultimately futile challenge.
Broadening the analysis
As part of the annual planning round, an analysis of forecast demand and capacity is undertaken – typically at an organisational level and based on historic values. However, by broadening this, there is an opportunity to derive far greater clarity on the size and nature of pressure points, enabling a more coherent plan for mitigating actions before the winter pressures take hold. Practically speaking, what’s required is first to expand demand and capacity planning to include the entire urgent and emergency care pathway. Next, the assumptions that have been used to underpin this initial model will require adjusting to reflect the actual observed demand and capacity requirements. The former action enables moderation of the pressures affecting capacity in the acute setting through community or other settings, while the latter provides a more accurate view of expected future pressures.
A second step that can be taken to help mitigate the effects of spiking winter demand is to identify actions that support improved intra-hospital flow. Ironically, it may be the reduced pressure on occupancy rates during the summer months that results in inadequacies not being highlighted. But if these failures are not remedied early, there is little time or capacity to address them during the demanding winter months.
Speeding up patient flow
So, what are the ‘must dos’? Great examples that quicken the patient flow through hospitals include: ensuring assessment
areas are fully staffed and that key clinical indicators are reviewed to ensure potential bottle necks are addressed; early morning reviews are undertaken of all patients by a senior clinician; patients ready for discharge are identified the evening before, plan for discharge medications early, and ensure discharge areas are set up appropriately.
Next, it’s important to strengthen operational management and governance. System resilience groups (SRGs) are the nationally prescribed forums responsible for delivery – however, most SRGs are not set up to manage operational pressures in real time across the pathway during winter. To rectify this, they should review their governance and establish operational subgroups with delegated authority to manage winter pressures proactively. It will be necessary to agree and monitor key performance indicators across the whole system in real time, identifying specific challenges in the pathway, and then to use the data sets this generates to extract the lessons that will help them with future planning decisions.
A ‘system reset’ after Christmas
While the above certainly aren’t silver bullet solutions, these are real actions that the NHS can begin implementing now to help make next winter less difficult. There’s one more thing that’s worth considering that won’t help with 2015-16 but will enhance the actions above for the following winter: a ‘system reset’ after Christmas.
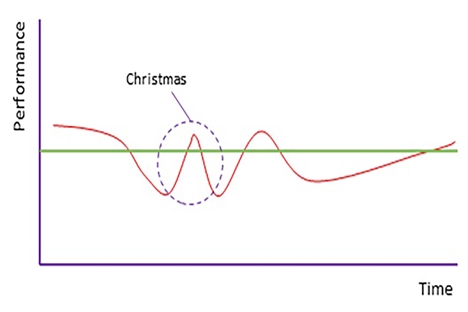
Past performance invariably shows a spike in effectiveness during the Christmas week, a notable blip in the significant underperformance that otherwise characterises winter – the Christmas ‘W’ (see graph above). During the first two weeks of the new year in 2017, SRGs could therefore focus on initiatives that support a maintained step change in delivery.
If the whole system can be engaged in such initiatives through participation from SRGs and their constituent parts, it should be possible to recognise immediate improvements in performance as the system recalibrates. Moreover, these improvements can be made sustainable as key learnings are identified, absorbed and acted on. Putting in place formal programmes to embed these across the system over February and March will allow still further improvements to be made through the summer period.
As already stated, there’s no simple fix to the challenges of winter, but the initiatives described above will help to form the foundations for improvement. Of course, each hospital and health system is different, and to ensure that any such improvements are sustainable, approaches must understand and tailor to the local challenges. Our experience would strongly suggest that such initiatives pay dividends in terms of reducing stress on the system, the care providers and, most importantly, the ability of our precious NHS to save lives.
Tell us what you think – have your say below or email [email protected]