Teachers, school nurses and GPs will be offered new NHS training to help them spot the early signs of eating disorders in children and young people, ensuring no child is left to “suffer in silence”.
The move follows a major overhaul of NHS eating disorder services after demand rose sharply in the years following the pandemic. NHS figures show the number of children and young people receiving specialist treatment has increased by two fifths, rising from 8,034 in 2019/20 to 11,174 in 2024/25.
New national NHS guidance, published today, represents the first major update to advice on children and young people with eating disorders since 2015. The guidance explicitly warns clinicians not to rely on body mass index (BMI) thresholds when deciding whether someone needs treatment, clamping down on what experts say is an outdated and potentially unsafe practice.
Instead, NHS clinicians are being advised to consider a broader range of indicators, including changes in behaviour, eating patterns, rapid weight loss, psychological distress and concerns raised by families, allowing earlier intervention before conditions worsen.
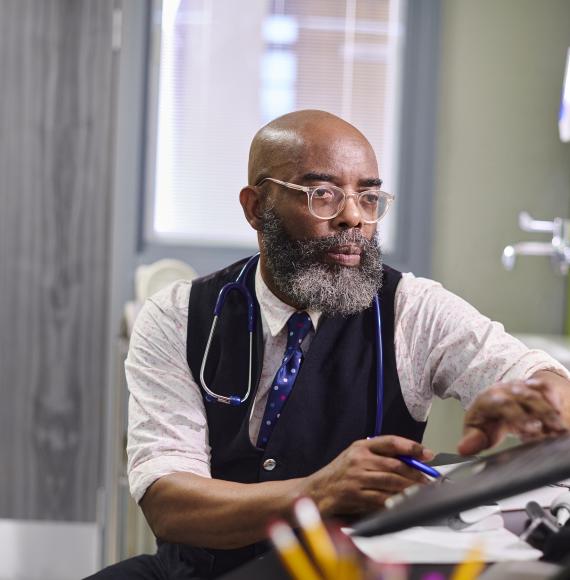
Under the new approach, online training will be rolled out to teachers, GPs and school nurses, helping professionals outside specialist services recognise warning signs and understand referral routes into NHS care. The training has been developed with support from the eating disorder charity Beat and the Royal College of Psychiatrists.
Every local area in England now has access to a specialist eating disorder service for children and young people, a dramatic shift from a decade ago when provision was limited to only a handful of regions. As a result of service expansion, children are now seen and offered treatment within an average of three weeks of referral for conditions such as anorexia nervosa, bulimia nervosa and binge eating disorder.
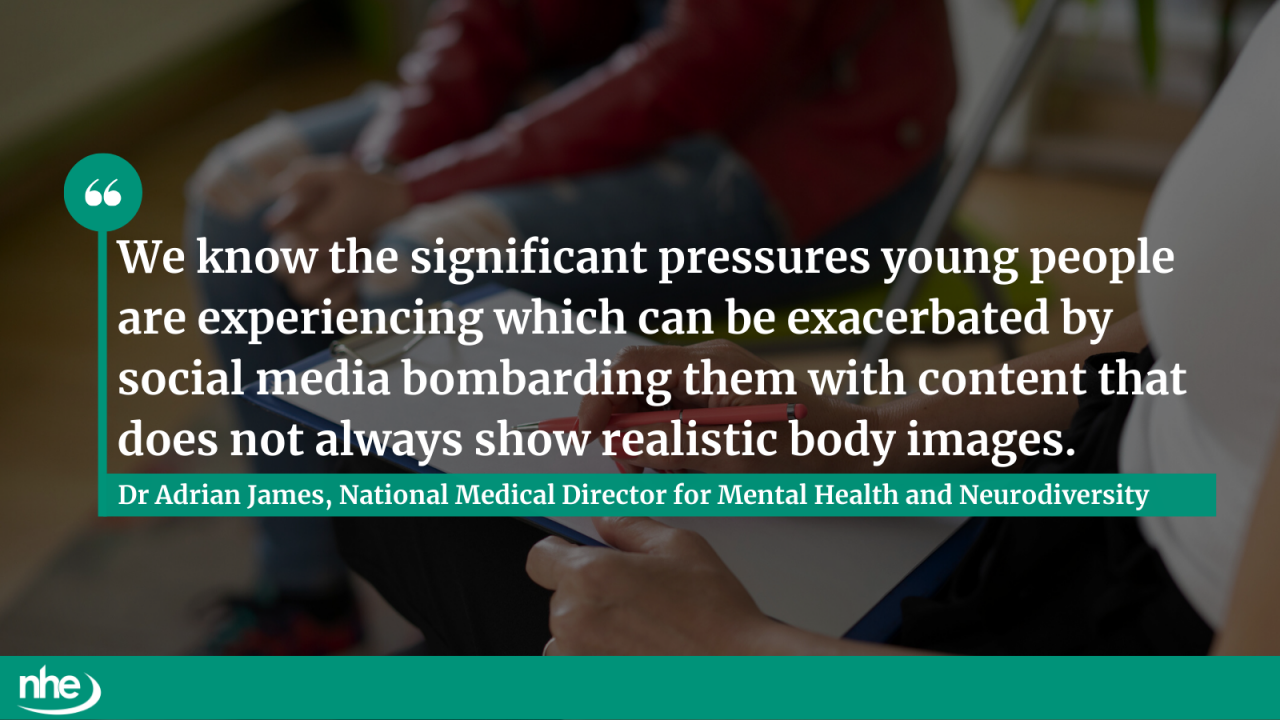
Dr Adrian James, NHS England’s National Medical Director for Mental Health and Neurodiversity, said:
“NHS staff have worked incredibly hard to transform eating disorder services over the last decade, but we are determined to ensure no child is left to suffer in silence.
“We know the significant pressures young people are experiencing which can be exacerbated by social media bombarding them with content that does not always show realistic body images.
“And we’re seeing the impact of that with growing numbers of young people turning to the NHS for eating disorder support, but it’s vital that everyone knows how to access this treatment which is why we will be offering training to teachers, GPs and school nurses to spot the signs and refer children for specialist help faster.
“So, if you or anyone you know is in need of support please contact your GP”.
The changes form part of the NHS’s 10 Year Health Plan, which prioritises providing care closer to home and intervening earlier to prevent young people becoming seriously unwell or needing hospital treatment.
Today’s guidance was co‑produced with clinicians, charities and professional bodies, reflecting wide‑ranging consultation and expert consensus. NHS leaders say the reforms represent a significant step forward in ensuring eating disorder care is timely, compassionate and evidence‑based.
Image credit: iStock